Bioengineered breast reconstruction and augmentation — dr. luba perry, phd — CEO, reconstruct bio.
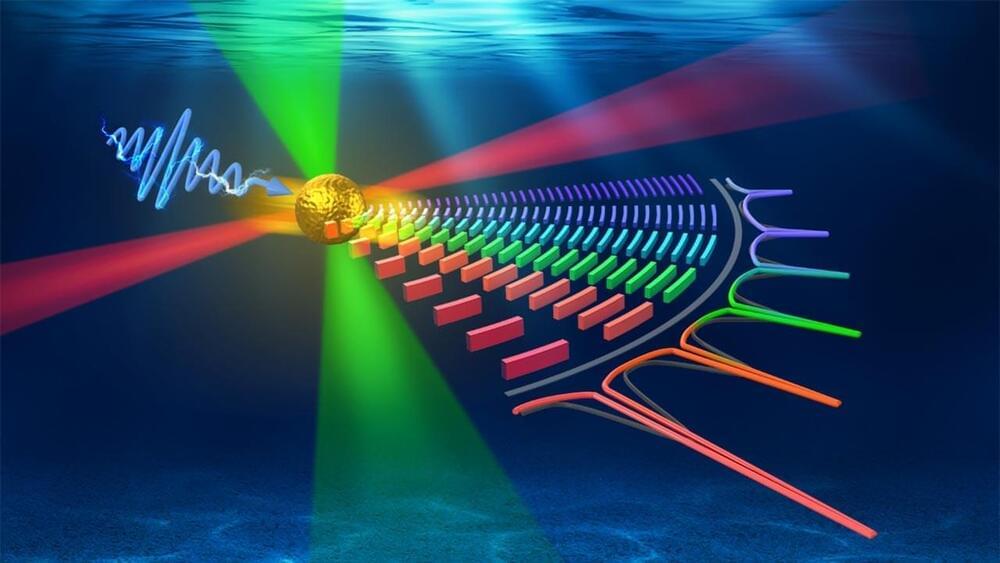
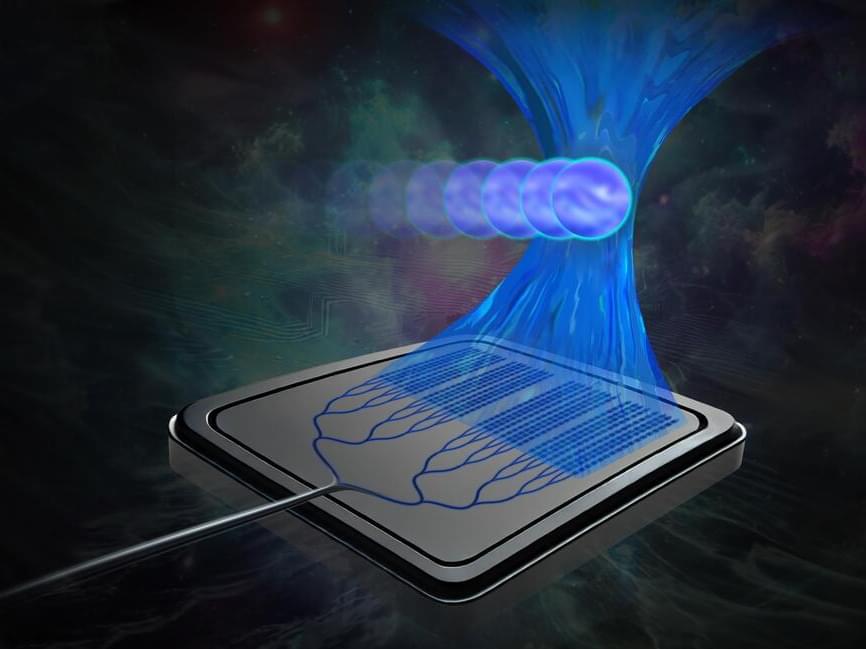
Dr. Luba Perry, Ph.D. is Co-Founder and CEO of ReConstruct Bio (https://wyss.harvard.edu/technology/r…), an innovative venture emerging from Harvard’s Wyss Institute (https://wyss.harvard.edu/team/advance…), aimed at redefining the fields of medical reconstruction and aesthetics with an initial application of their groundbreaking technology on breast reconstruction and augmentation. With a multidisciplinary team of experts, the ReConstruct Bio team has developed the BioImplant—a living, bioengineered tissue created from the patient’s own cells, to provide safer, more natural alternative to current standards, which are often associated with significant drawbacks and health concerns.
Dr. Perry also serves as a Senior Scientist at the Wyss Institute for Biologically Inspired Engineering working at the 3D Organ Engineering Initiative since 2018 and is leading a Wyss Validation Project aiming to fabricate vascularized functional tissues for transplantation. Her interest is in tissue and organ engineering, focusing on vascularization and implantation studies utilizing complex surgical models.
Dr. Perry’s background is in molecular biology, pharmacology, and biomedical engineering, with a Bachelor of Science — BS, Biology, Master of Science — MS, Molecular Pharmacology, and a Doctor of Philosophy — PhD, Biotechnology, all from Technion — Israel Institute of Technology. She also has industry experience in a vascular gene therapy company (MGVS, now VESSL Therapeutics).
#LubaPerry #Harvard #WyssInstitute #ReConstructBio #Aesthetics #3DOrganEngineering #BreastReconstruction #BreastAugmentation #Vascularization #Innervation #Fat #AdiposeTissue #BreastImplants #Organogenesis #OrganEngineering #TissueEngineering #Bioengineering #Organs #Tissues #MolecularPharmacology #Breasts #Nipples.