We move thanks to coordination among many skeletal muscle fibers, all twitching and pulling in sync. While some muscles align in one direction, others form intricate patterns, helping parts of the body move in multiple ways.
In recent years, scientists and engineers have looked to muscles as potential actuators for “biohybrid” robots—machines powered by soft, artificially grown muscle fibers. Such bio-bots could squirm and wiggle through spaces where traditional machines cannot. For the most part, however, researchers have only been able to fabricate artificial muscle that pulls in one direction, limiting any robot’s range of motion.
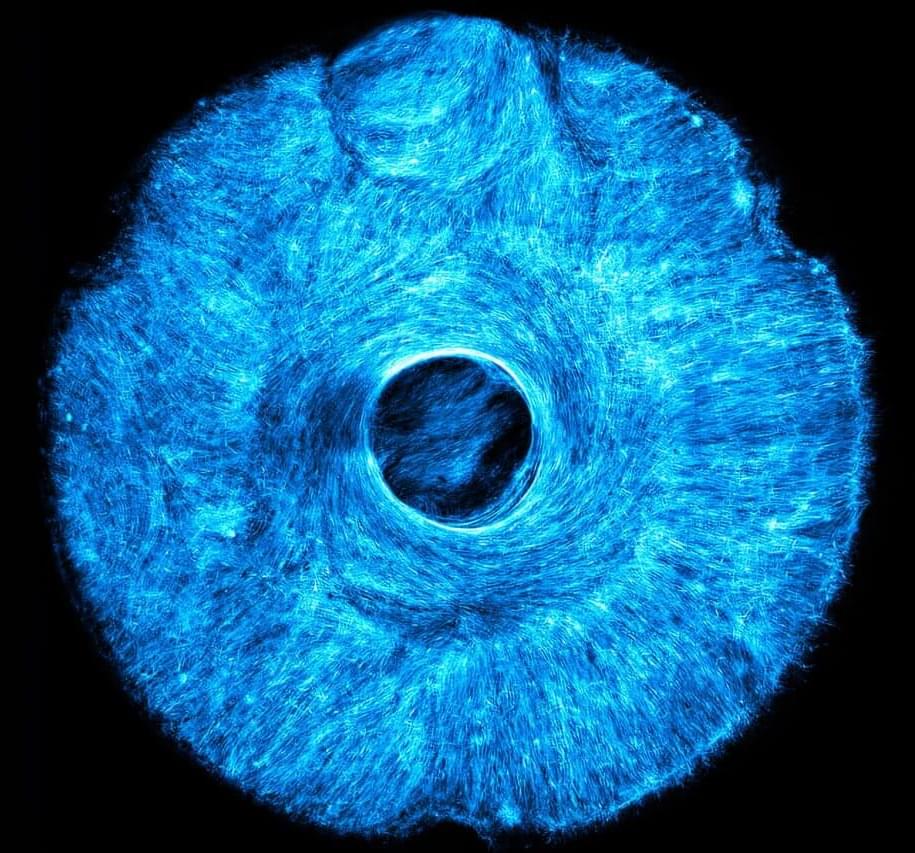
Now MIT engineers have developed a method to grow artificial muscle tissue that twitches and flexes in multiple coordinated directions. As a demonstration, they grew an artificial, muscle-powered structure that pulls both concentrically and radially, much like how the iris in the human eye acts to dilate and constrict the pupil.