A little over a year ago, Joseph Coates was told there was only one thing left to decide. Did he want to die at home, or in the hospital?
Coates, then 37 and living in Renton, Wash., was barely conscious. For months, he had been battling a rare blood disorder called POEMS syndrome, which had left him with numb hands and feet, an enlarged heart and failing kidneys. Every few days, doctors needed to drain liters of fluid from his abdomen. He became too sick to receive a stem cell transplant — one of the only treatments that could have put him into remission.
“I gave up,” he said. “I just thought the end was inevitable.”
But Coates’s girlfriend, Tara Theobald, wasn’t ready to quit. So she sent an email begging for help to a doctor in Philadelphia named David Fajgenbaum, whom the couple met a year earlier at a rare disease summit.
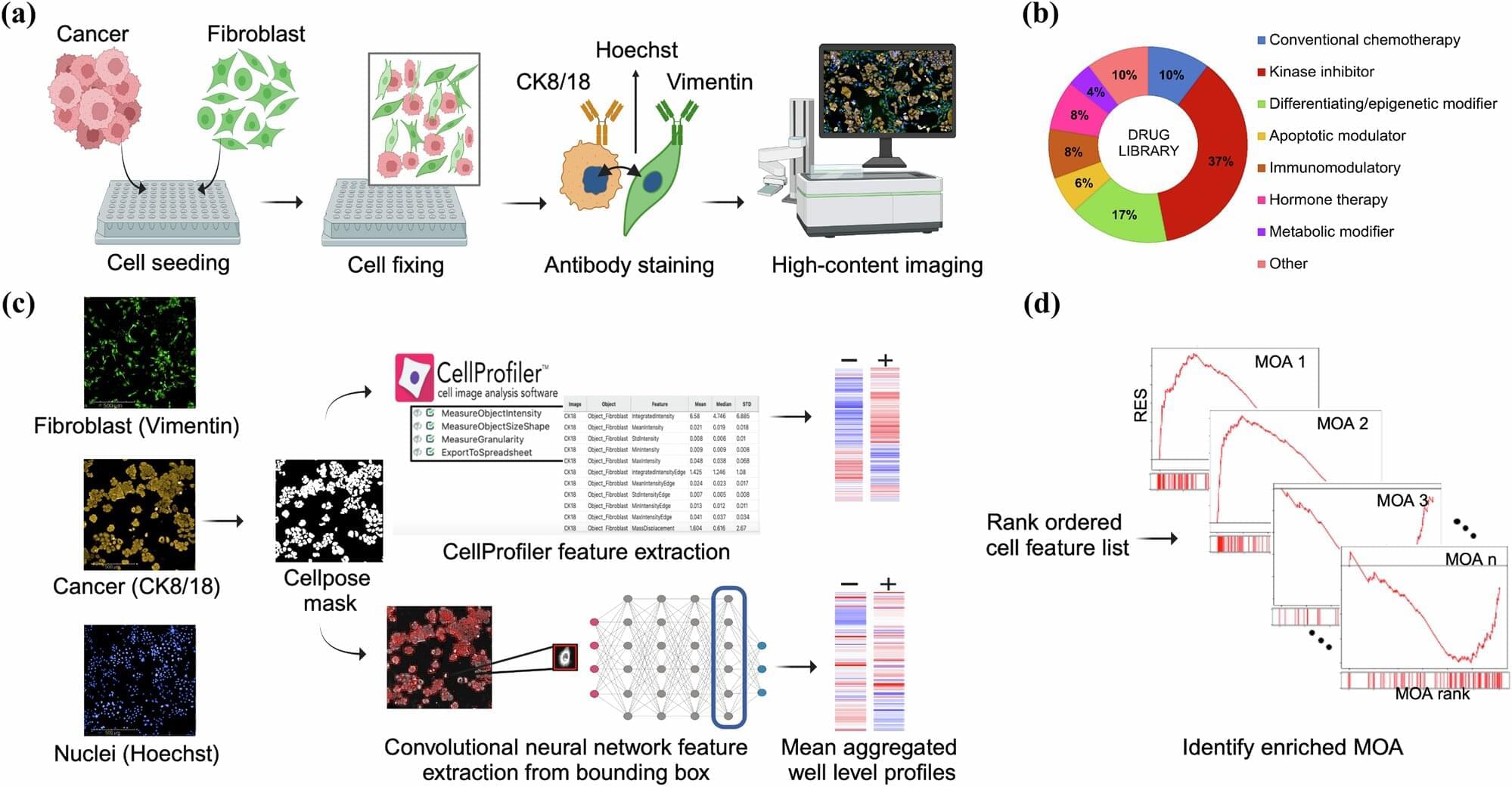
Scientists are using machine learning to find new treatments among thousands of old medicines.