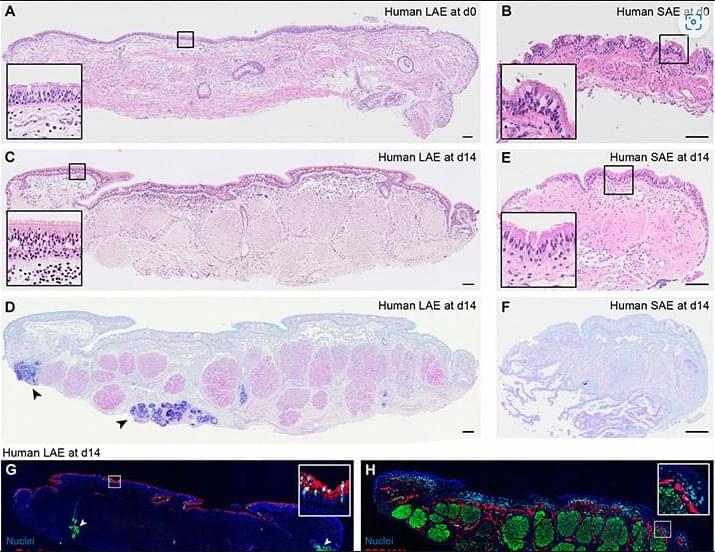
Ex vivo models capture the cellular and functional richness of respiratory tract tissues and enable study of viral pathogenesis.
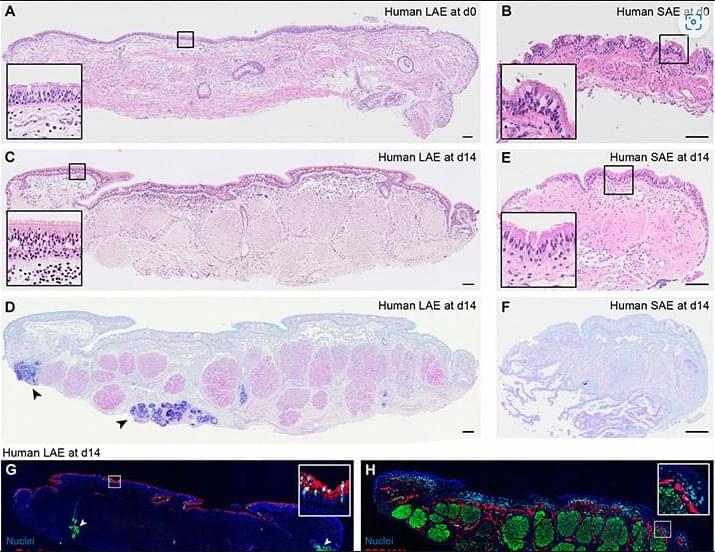
Self-propulsion enzymatic nanomotors have shown tremendous potential in the field of diagnostics. In a study led by Wang and coworkers, nanoenzyme-driven cup-shaped nanomotors were designed for enhanced cell penetration and synergistic photodynamic/thermal treatments under single near-infrared laser irradiation. By combining the concepts of self-propulsion enzymatic nanomotors and synergistic dual-modal therapy, this work provides a new idea and tool for the application of nanomotors in the biomedical field.
1st with ALS. 1st nonverbal.
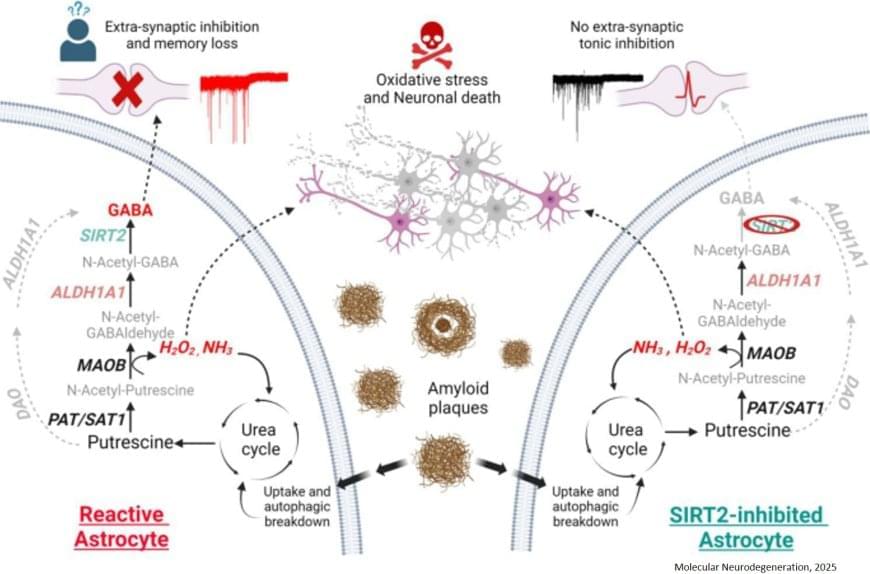
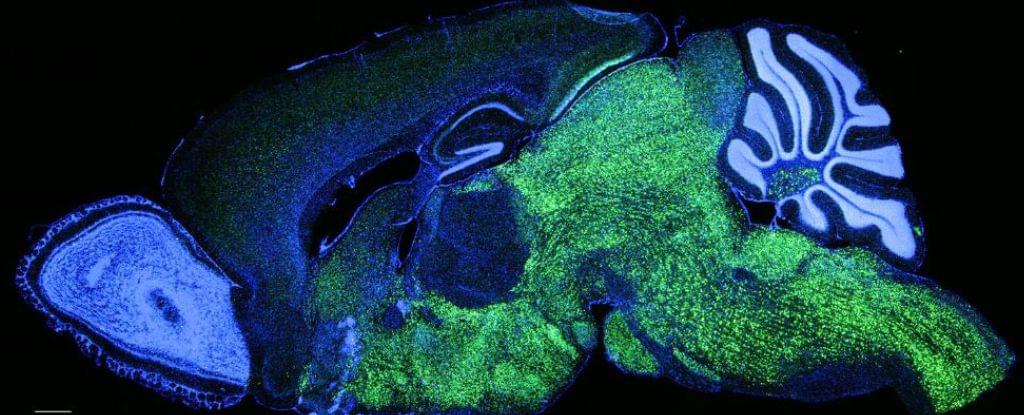
A research team has identified a previously unknown enzyme, SIRT2, that plays a key role in memory loss associated with Alzheimer’s disease (AD). The study provides critical insights into how astrocytes contribute to cognitive decline by producing excessive amounts of the inhibitory neurotransmitter GABA.
Astrocytes, once thought to only support neurons, are now known to actively influence brain function. In Alzheimer’s disease, astrocytes become reactive, meaning they change their behavior in response to the presence of amyloid-beta (Aβ) plaques, a hallmark of the disease. While astrocytes attempt to clear these plaques, this process triggers a harmful chain reaction. First, they uptake them via autophagy and degrade them by the urea cycle, as discovered in previous research. However, this breakdown results in the overproduction of GABA, which dampens brain activity and leads to memory impairment. Additionally, this pathway generates hydrogen peroxide (H2O2), a toxic byproduct that causes further neuronal death and neurodegeneration.
The research team set out to uncover which enzymes were responsible for excessive GABA production, hoping to find a way to selectively block its harmful effects without interfering with other brain functions. Using molecular analysis, microscopic imaging, and electrophysiology, the researchers identified SIRT2 and ALDH1A1 as critical enzymes involved in GABA overproduction in Alzheimer’s-affected astrocytes.
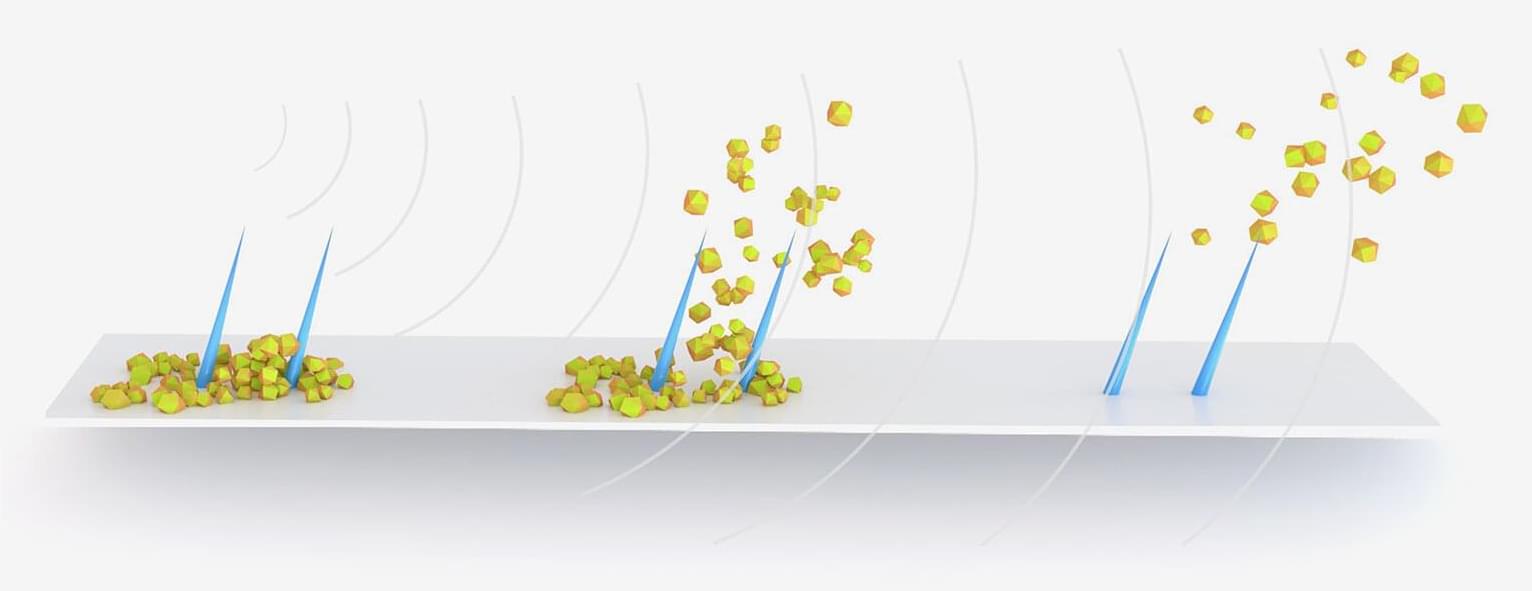
Urinary stents and catheters are implanted medical tubes that are widely used in human and veterinary medicine to drain urine to/from the bladder. Ureteral stents are used when the ureter, the duct between the kidney and bladder, is blocked by tumors, pregnancy, stones or anatomical narrowing.
Biofilm, produced by bacteria, and crystalline deposits, called encrustation, grow on the inner and outer walls of such stents and catheters soon after implantation and are among the main causes of failure of these devices because they lead to painful blockages and urinary infections.
To mitigate these issues, urinary stents and catheters therefore must be replaced every two to six months, which not only considerably restricts the quality of life of those affected but also leads to high hospital load and costs.
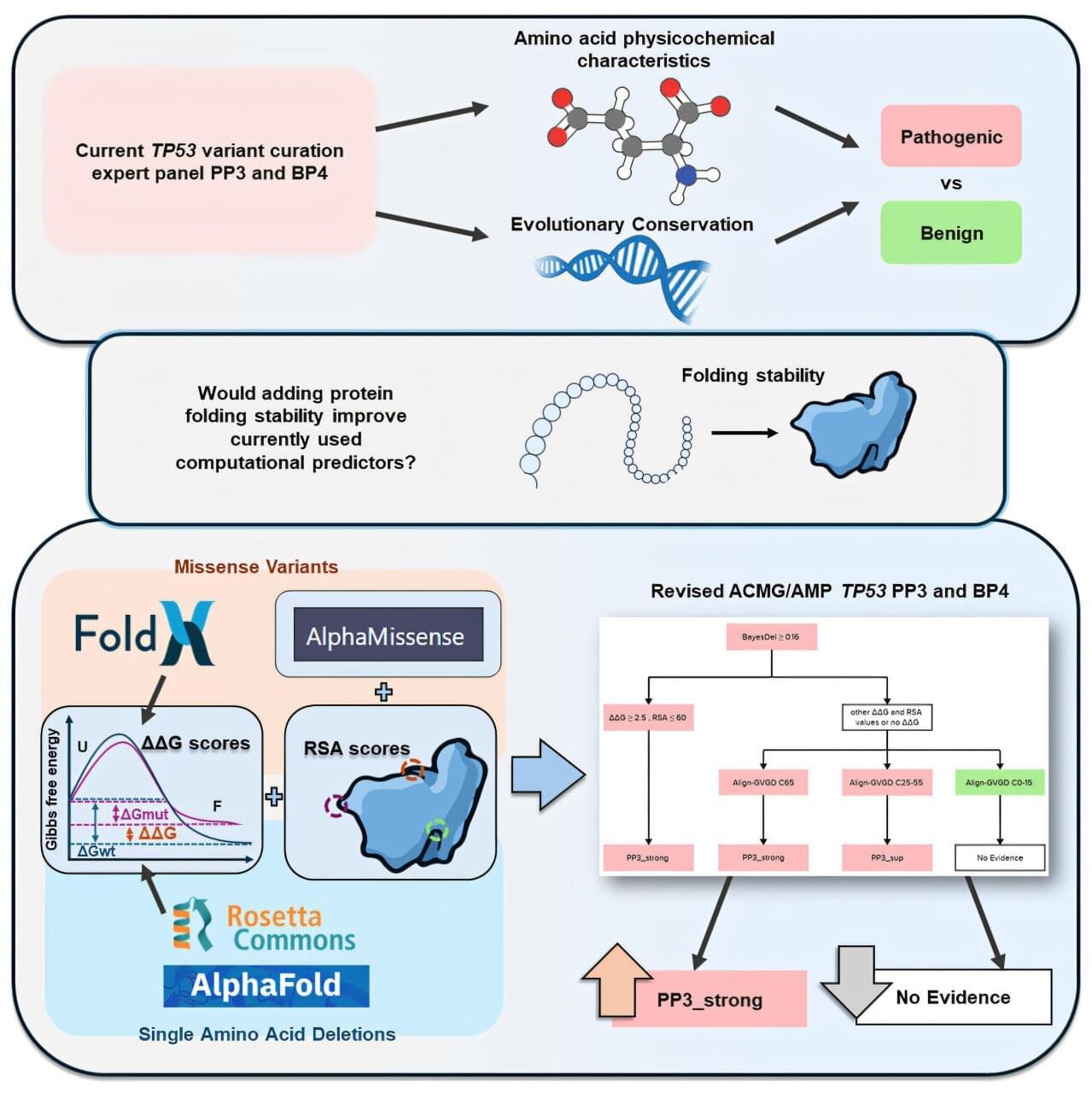
QIMR Berghofer-led research has shown that new advanced computational prediction tools can improve the accuracy of genetic testing for families affected by an inherited condition that significantly increases their risk of developing cancer, paving the way to better targeted care.
The findings have been published in the American Journal of Human Genetics alongside complementary studies by international collaborators, which together show how incorporating the new computational biology tools with existing modeling methods improved the predictive power of genetic test results.
Computational tools are used to predict if and how a genetic variant is likely to impact the function of the protein encoded by the gene.
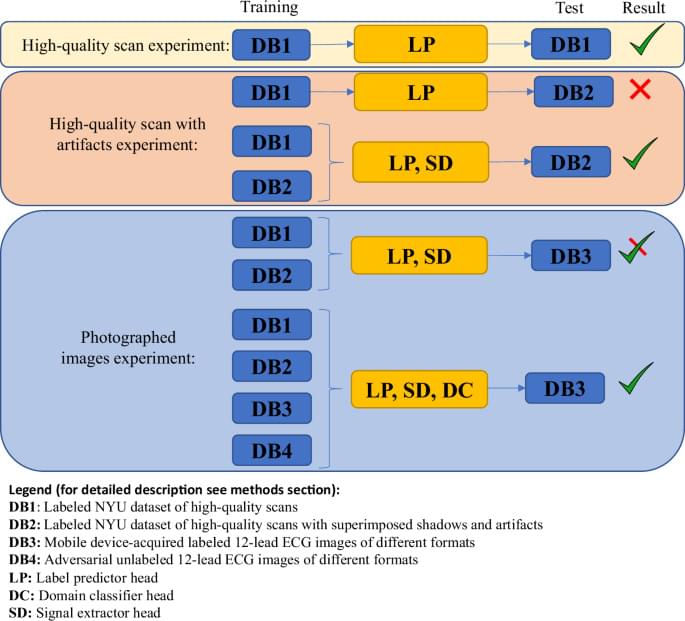
Gliner, V., Levy, I., Tsutsui, K. et al. Clinically meaningful interpretability of an AI model for ECG classification. npj Digit. Med. 8, 109 (2025). https://doi.org/10.1038/s41746-025-01467-8
