Neuroblastoma, a pediatric cancer of the nervous system, remains the leading cause of cancer-related death in young children, particularly when the disease has spread. Despite aggressive treatment regimens that include surgery, radiation, chemotherapy, and immunotherapy, metastatic neuroblastoma often proves incurable, largely because the cancer can evade or resist standard therapies.
One approach, known as differentiation therapy, attempts to coax immature neuroblastoma cells into developing into mature, noncancerous nerve cells. But current differentiation treatments, such as retinoic acid (RA), are only partially effective: many patients fail to respond, and nearly half of those who do eventually relapse due to resistance.
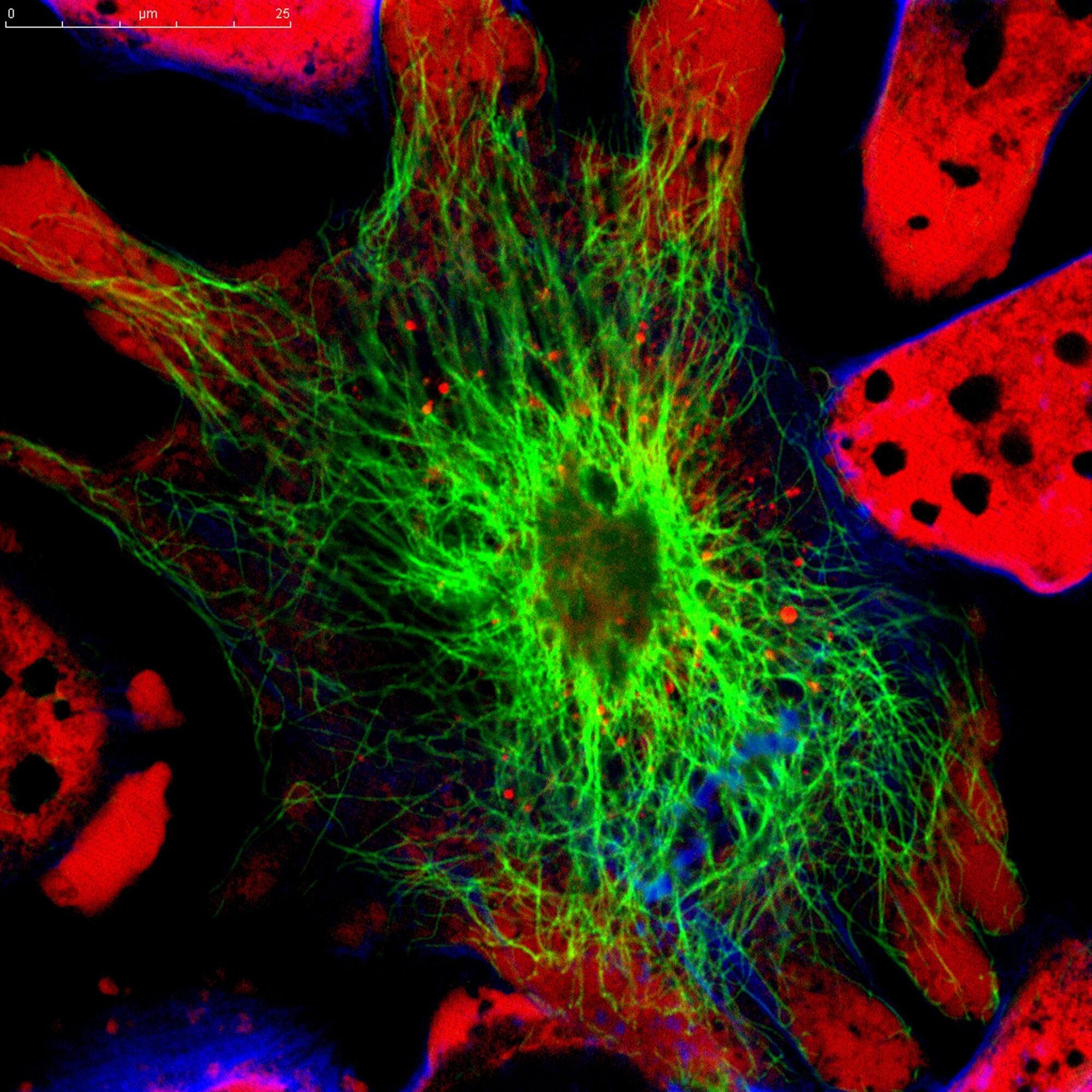
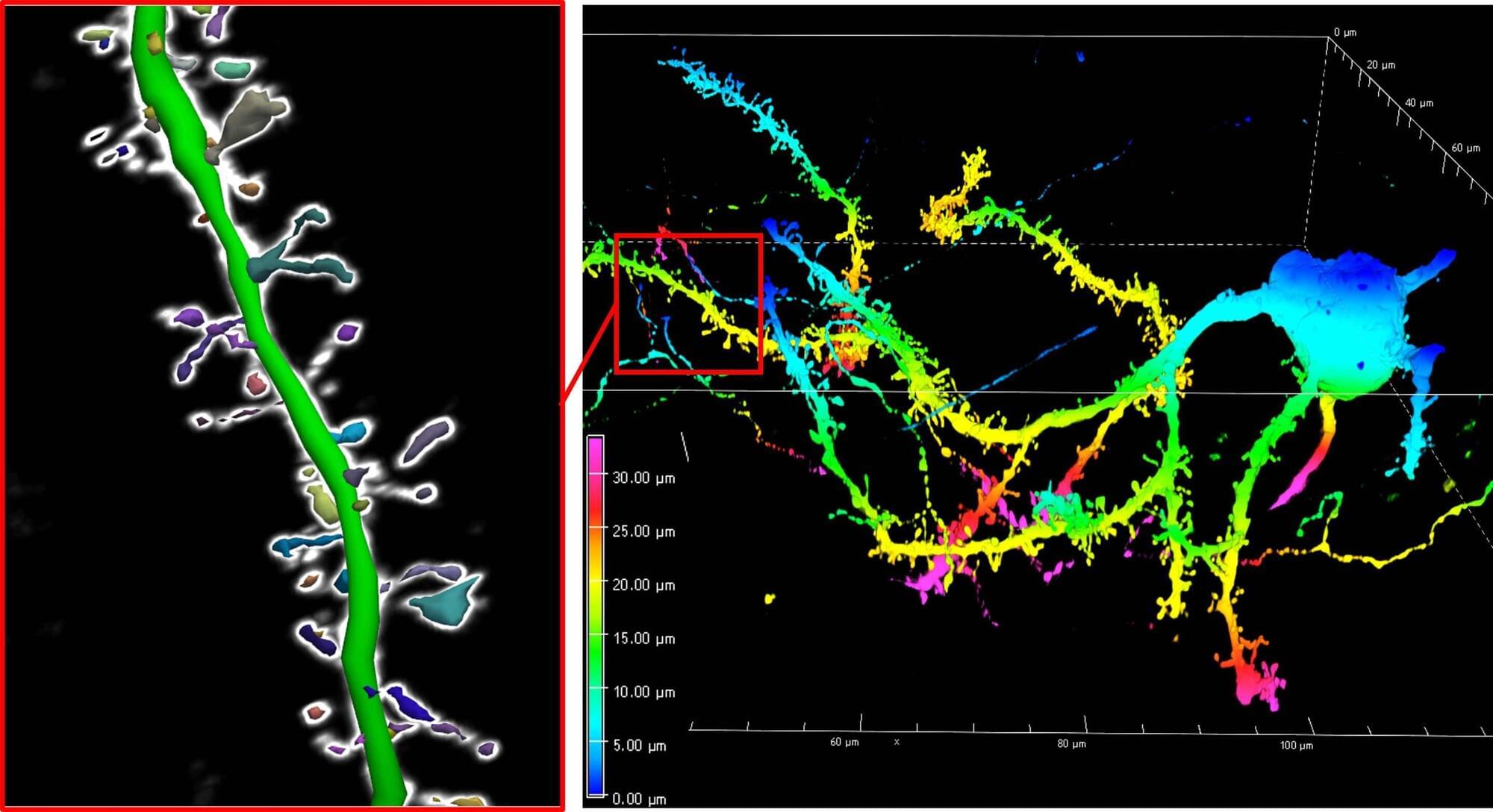
Now, researchers at Karolinska Institutet and Lund University in Sweden have identified an alternative approach—targeting the antioxidant enzymes PRDX6 and GSTP1—that may sidestep the limitations of RA. The study, “Combined targeting of PRDX6 and GSTP1 as a potential differentiation strategy for neuroblastoma treatment,” published in Proceedings of the National Academy of Sciences, shows that dual inhibition of these enzymes not only kills some neuroblastoma cells but also transforms others into healthy, active neurons.