Second Sight Medical (NSDQ: EYES) today announced the first trial implantation of its Orion cortical visual prosthesis system and updated on implantations of its Argus device and enrollment in an upcoming study.
The first implantation procedure was performed late last month by Dr. Nader Pouratian at the Ronald Reagan UCLA Medical Center, the Sylmar, Calif.-based company said, as part of an FDA-cleared feasibility trial it won approval to launch last November.
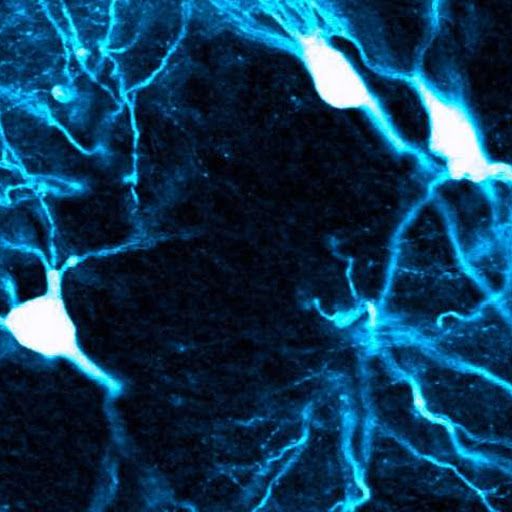
The Orion cortical visual prosthesis system is designed to convert images captured by a miniature video camera, mounted on a patient’s glasses, into a series of electrical pulses which are transmitted wirelessly to an array of electrodes on the surface of the individual’s visual cortex.