Reading human DNA used to take laboratories, a pile of cash and a long time.


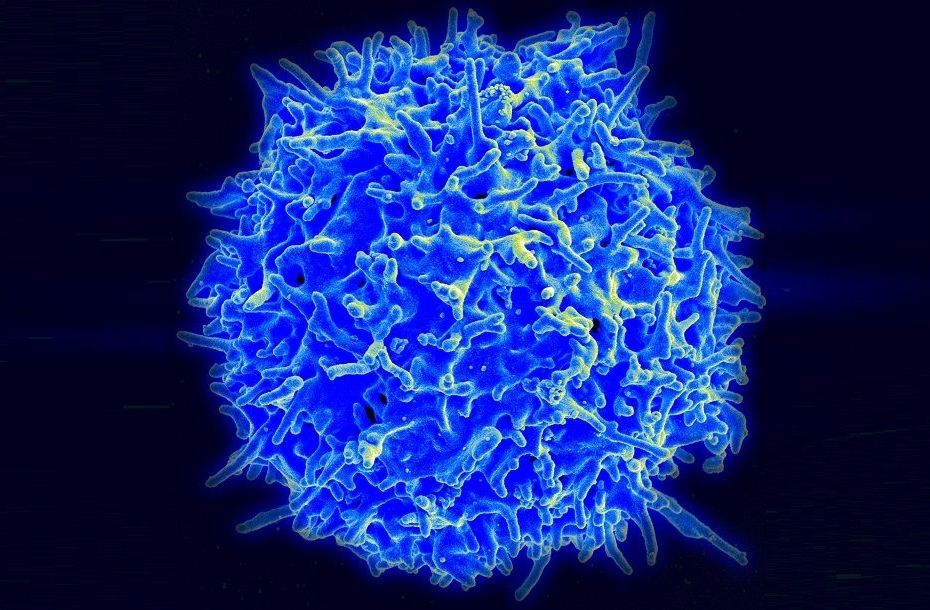
This revolutionary gene modified T cell therapy is bearing fruit in treating a type of lymphoma, a resistant form of cancer.
Summary: After years of effort, this revolutionary gene-modified T cell therapy is bearing fruit in treating a type of lymphoma, a resistant form of cancer. [This article first appeared on the website LongevityFacts.com. Author: Brady Hartman. ]
Thirty-seven-year-old Nick Asoian of Denver unsuccessfully fought Hodgkin’s Lymphoma using conventional cancer treatments for two years. In 2008, while in New Zealand for a ski race, Nick was diagnosed with Hodgkin’s Lymphoma. Two bone marrow transplants and two years of chemotherapy combined with radiation therapy didn’t bring his cancer to heel.
Then, a few years ago the avid skier got wind of clinical trial using T cell therapy at the Center for Cell and Gene Therapy at the Baylor College of Medicine in Texas. After speaking with Dr. Bollard and Vicky Torrano, the physicians conducting the trial, Asoian decided to give it a shot.

By Ben Hirschler
LONDON (Reuters) — Chinese scientists have cloned monkeys using the same technique that produced Dolly the sheep two decades ago, breaking a technical barrier that could open the door to copying humans.
Zhong Zhong and Hua Hua, two identical long-tailed macaques, were born eight and six weeks ago, making them the first primates — the order of mammals that includes monkeys, apes and humans — to be cloned from a non-embryonic cell.

The ocean is crowded. As many as 10 million viruses can be found squirming in a single millilitre of its water, and it turns out they have friends we never even knew about.
Scientists have discovered a previously unknown family of viruses that dominate the ocean and can’t be detected by standard lab tests. Researchers suspect this viral multitude may already exist outside the water — maybe even inside us.
“We don’t think it’s ocean-specific at all,” says environmental microbiologist Martin Polz from MIT.
Einstein’s secret to an incredibly intelligent brain may be in part to how well his brain aged…
Samples of his brain revealed he was missing a protein Lipofuscin, a not so well understood compound which contains lipid residues of lysosomal digestion that accumulates in the brain liver kidney, heart muscle, retina, adrenals, nerve cells, and ganglion cells.
Lipofuscin busting drugs could have a lot of potential for anti-aging therapies for the future.
The debate over telomeres length is now back in the spotlight… Here is a brief review of the top articles on telomere length, telomerase and human diseases such as cancer…
A review of the top articles on telomerase and telomere length which play a role in the chronic diseases of aging, such as cancer.
Robots are already changing jobs as an endless array of robots enter our everyday lives. From trucking to service work to high-end jobs like doctors and lawyers, this documentary explores how robotics and artificial intelligence are changing the workplace.
AJ+‘s documentary series on automation explores how advancements in artificial intelligence, robotics, machine learning and automated vehicles will affect jobs, cities and inequality. From trucking to radiology, new technology is already changing white collar and blue collar occupations, reshaping cities and concentrating wealth in the hands of the few. Robots are taking over the world as companies like Tesla, Amazon, Uber and Google are using robots to automate.
Subscribe for more videos:
Like us on Facebook: https://www.facebook.com/ajplusenglish
Download the AJ+ app at http://www.ajplus.net/
Follow us on Twitter: https://twitter.com/ajplus


Imagine being able to see three times better than 20/20 vision without wearing glasses or contacts — even at age 100 or more — with the help of bionic lenses implanted in your eyes.
Dr. Garth Webb, an optometrist in British Columbia who invented the Ocumetics Bionic Lens, says patients would have perfect vision and that driving glasses, progressive lenses and contact lenses would become a dim memory as the eye-care industry is transformed.

As we age, our bodily functions begin to deteriorate. To some extent, our bodies can cope with these unwelcome changes, but after age 35, some of them become visible. For us living in a world where youth and physical attractiveness are considered an advantage, this gradual loss of young looks can be painful – or maybe even scary, if we don’t know a way to slow down or reverse it.
It is not that physical attractiveness is a value per se for me, but I often hear people say that someone promoting longevity technologies should set a good example; wrinkles, dull skin and hair, and a bloated figure discredit not only the activist but the movement as a whole.
So, I keep an eye on what is going on in the field of aesthetic medicine – especially when it comes close to and crosses with rejuvenation biotechnologies. Last week, I went to one of the flagship research organizations in Moscow – the Human Stem Cells Institute – to interview Dr. Vadim Zorin, the head of the SPRS-therapy project and the developer of a unique approach to skin rejuvenation.