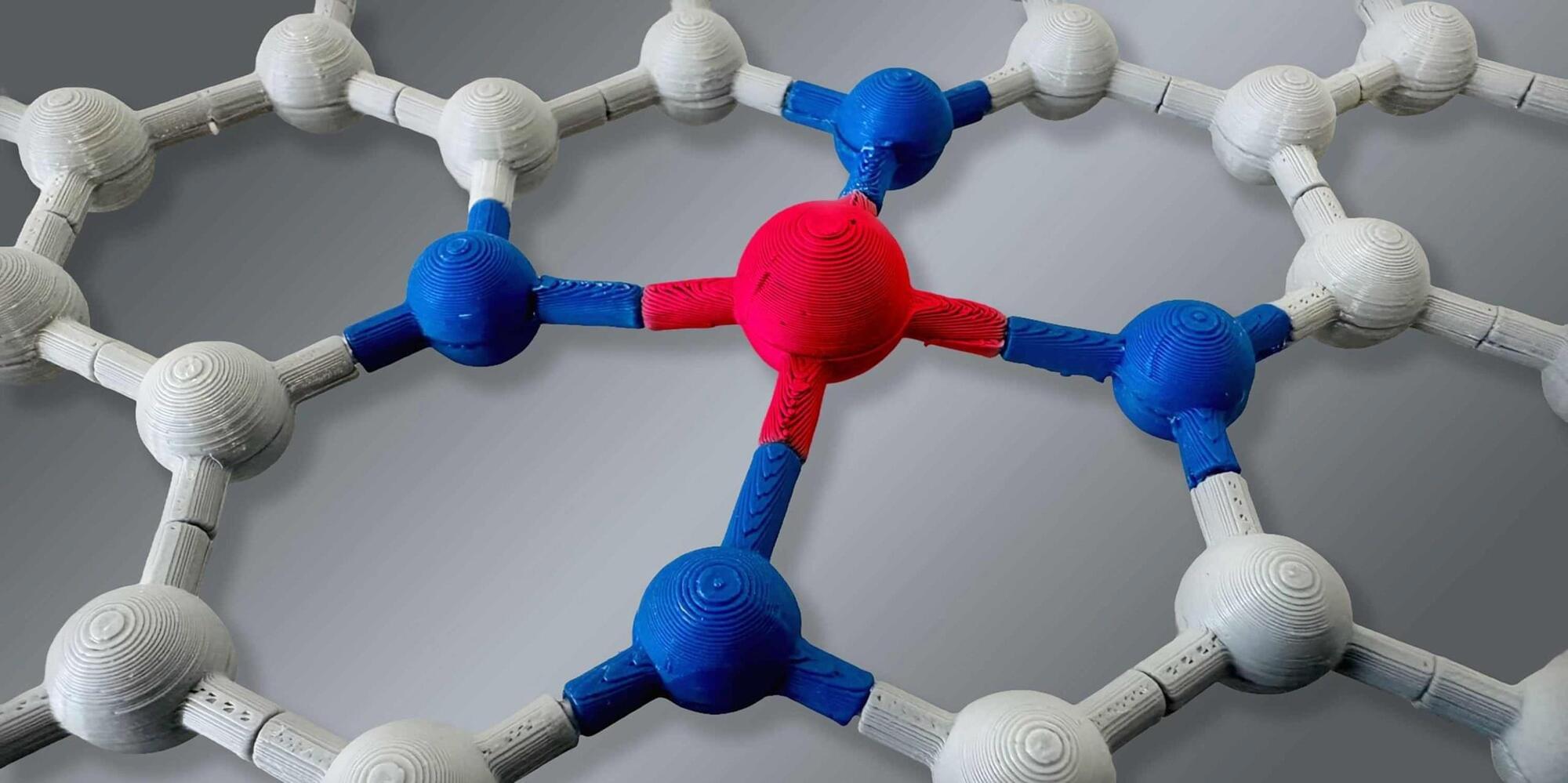
Landmark research on MCL-1, a critical protein that is an attractive target for cancer drug development, helps explain why some promising cancer treatments are causing serious side effects, and offers a roadmap for designing safer, more targeted therapies.
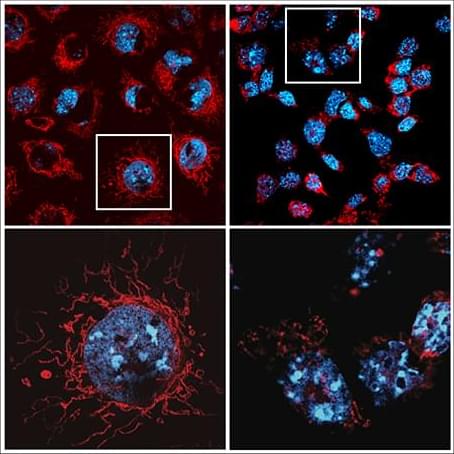
The WEHI-led discovery, published in Science, has uncovered a critical new role for MCL-1, revealing it not only prevents cell death but also provides cells with the energy they need to function.
The findings reshape our understanding of how cells survive and thrive, with implications for both cancer treatment and developmental biology.