There so sweet, just being around a dog is pure love & happiness!
Researchers found a lower risk of cardiovascular disease in owners of dogs, especially hunting breeds.

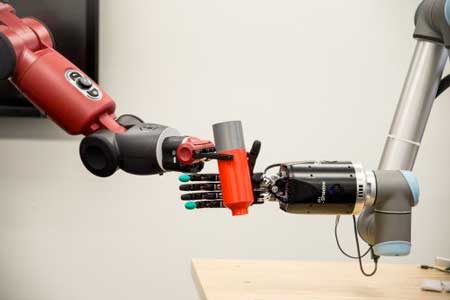
The sense of touch is often taken for granted. For someone without a limb or hand, losing that sense of touch can be devastating. While highly sophisticated prostheses with complex moving fingers and joints are available to mimic almost every hand motion, they remain frustratingly difficult and unnatural for the user. This is largely because they lack the tactile experience that guides every movement. This void in sensation results in limited use or abandonment of these very expensive artificial devices. So why not make a prosthesis that can actually feel its environment?
That is exactly what an interdisciplinary team of scientists from Florida Atlantic University and the University of Utah School of Medicine aims to do. They are developing a first-of-its-kind bioengineered robotic hand that will grow and adapt to its environment. This living robot will have its own peripheral nervous system directly linking robotic sensors and actuators. FAUs College of Engineering and Computer Science is leading the multidisciplinary team that has received a four-year, $1.3 million grant from the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health for a project titled Virtual Neuroprosthesis: Restoring Autonomy to People Suffering from Neurotrauma.

Interesting article about the longevity work of my friend James Clement in The New York Times: https://nyti.ms/2hw8W32 #transhumanism
James Clement has scoured the globe for supercentenarians, aged 110 and older, willing to contribute their genomes to a rare scientific cache.

It’s all a question of money. We should come up with enough money for funding this so that we can clone a perfect genetic match of every organ in the body by 2025. It will solve the organ shortage issue, and nip the illegal black market organ industry in the bud.
The FDA said it is looking into “regenerative medicine.”

Today, we take a look at three key emerging technologies that might add extra healthy years to your life by addressing the aging processes directly to prevent or delay age-related diseases.
Senolytics – Removing aged dysfunctional cells to promote tissue regeneration
As we age, increasing amounts of our cells enter into a state known as senescence. Normally, these cells destroy themselves by a self-destruct process known as apoptosis and are disposed of by the immune system. Unfortunately, as we age, increasing numbers of these cells evade apoptosis and linger in the body.
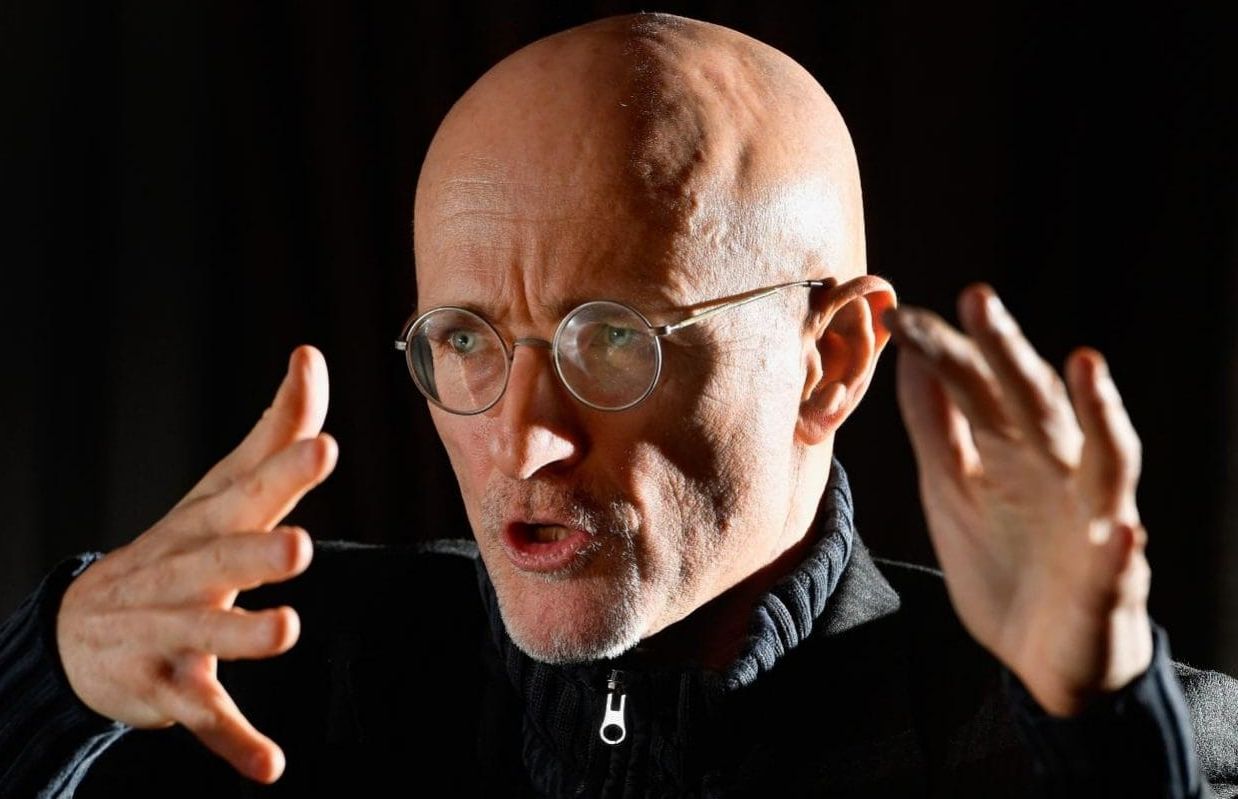
T he world’s first human head transplant has been carried out on a corpse in China in an 18-hour operation that showed it was possible to successfully reconnect the spine, nerves and blood vessels.
At a press conference in Vienna on Friday morning, Italian Professor Sergio Canavero, director of the Turin Advanced Neuromodulation Group, announced that a team at Harbin Medical University had “realised the first human head transplant” and said an operation on a live human will take place “imminently”.
The operation was carried out by a team led by Dr Xiaoping Ren, who last year successfully grafted a head onto the body of a monkey.
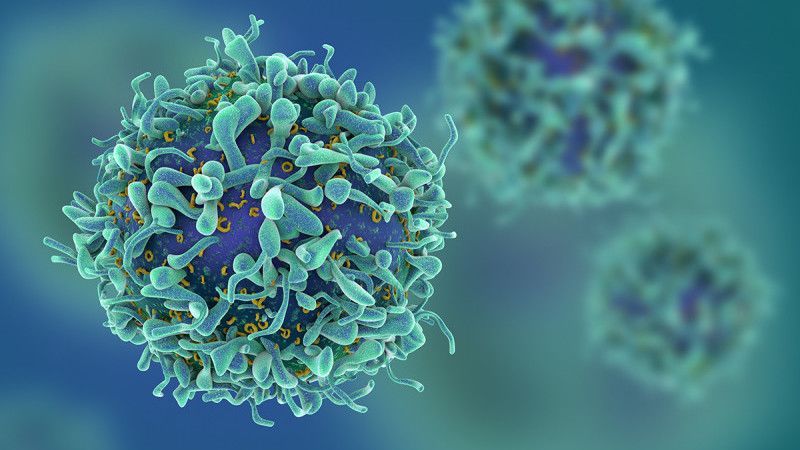
On Wednesday—for only the second time—the Food and Drug Administration approved a cutting-edge therapy that genetically modifies a patient’s blood cells in order to attack cancer. This time the therapy, known as CAR T-cell therapy, is designed to treat aggressive non-Hodgkin lymphoma.
In August, the FDA approved the first CAR T-cell therapy, for a drug called Kymriah designed for children and young adults whose leukemia doesn’t respond to standard treatments. The FDA’s approval of Yescarta, manufactured by Kite Pharma, comes just a few months after its first approval—an indication of just how quickly the field of immunotherapy is moving. Several other companies also have CAR-T therapies in the works.
There are many benefits to exercise and how it can reduce the impact of the aging process. We have previously talked about how even a moderate amount of gentle exercise, such as walking, dancing, and strength training, can improve health and reduce mortality.
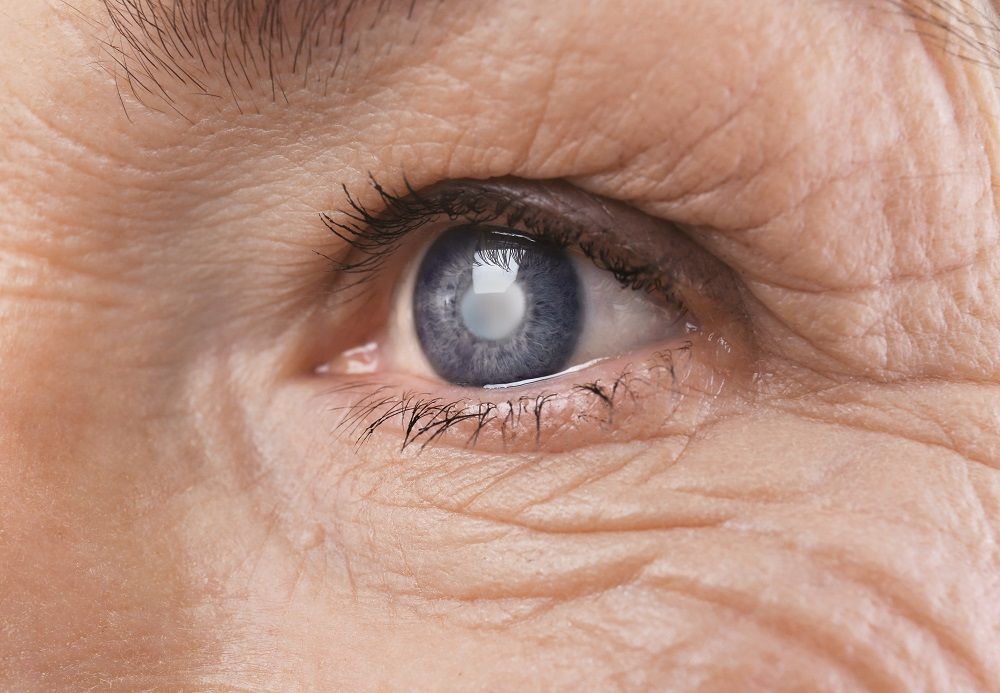
New research suggests that even moderate levels of physical activity can reduce glaucoma, one of the leading causes of blindness in the United States, and which is most prevalent among the elderly.
The data presented by UCLA researchers at the 121st Annual Meeting of the American Academy of Ophthalmology showed that the most physically active people involved in a recent study have a 73 percent reduced risk of developing glaucoma compared to the least active.

Every so often when talking about aging and eradicating age-related diseases someone will say there are other more important things that must be solved before we earn the right to live healthy and longer lives.
When you discuss any major issue, sooner or later someone will say it: there are more urgent issues than whatever it is you’re advocating for. Sometimes it may be true; other times, and probably most of the time, it’s a logical fallacy known as appeal to worse problems (or “not as bad as”, or even “fallacy of relative privation”).
For example, say you’ve got two issues, A and B, that cannot possibly be both dealt with at the same time; if A is life-threatening and B isn’t, well, then I think it’d make sense to reply “there are more urgent issues” to whoever suggests B should be taken care of first. However, all too often, this answer is abused to play down the importance of a problem that doesn’t happen to be one’s personal favourite—and yes, I’ve seen this happen with rejuvenation therapies.

To mark the letter’s 25th anniversary, researchers have issued a bracing follow-up. In a communique published Monday in the journal BioScience, more than 15,000 scientists from 184 countries assess the world’s latest responses to various environmental threats. Once again, they find us sorely wanting.
In 1992, scientists warned humanity about a host of impending ecological disasters. A quarter-century later, most of them have gotten worse.