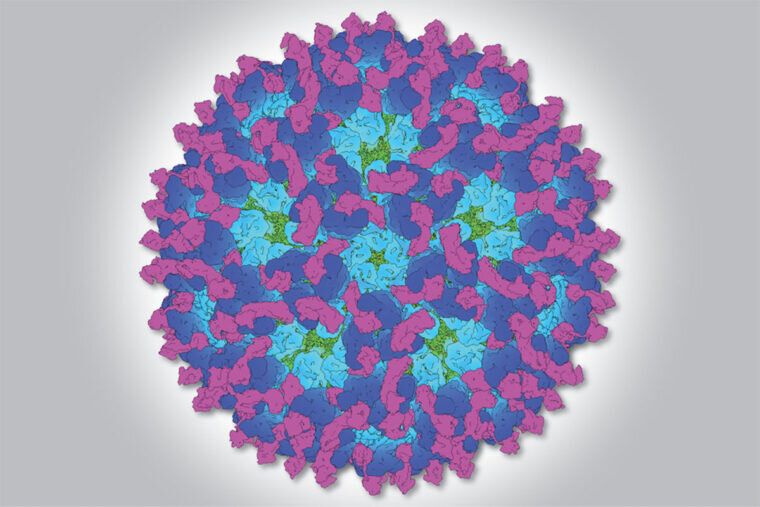
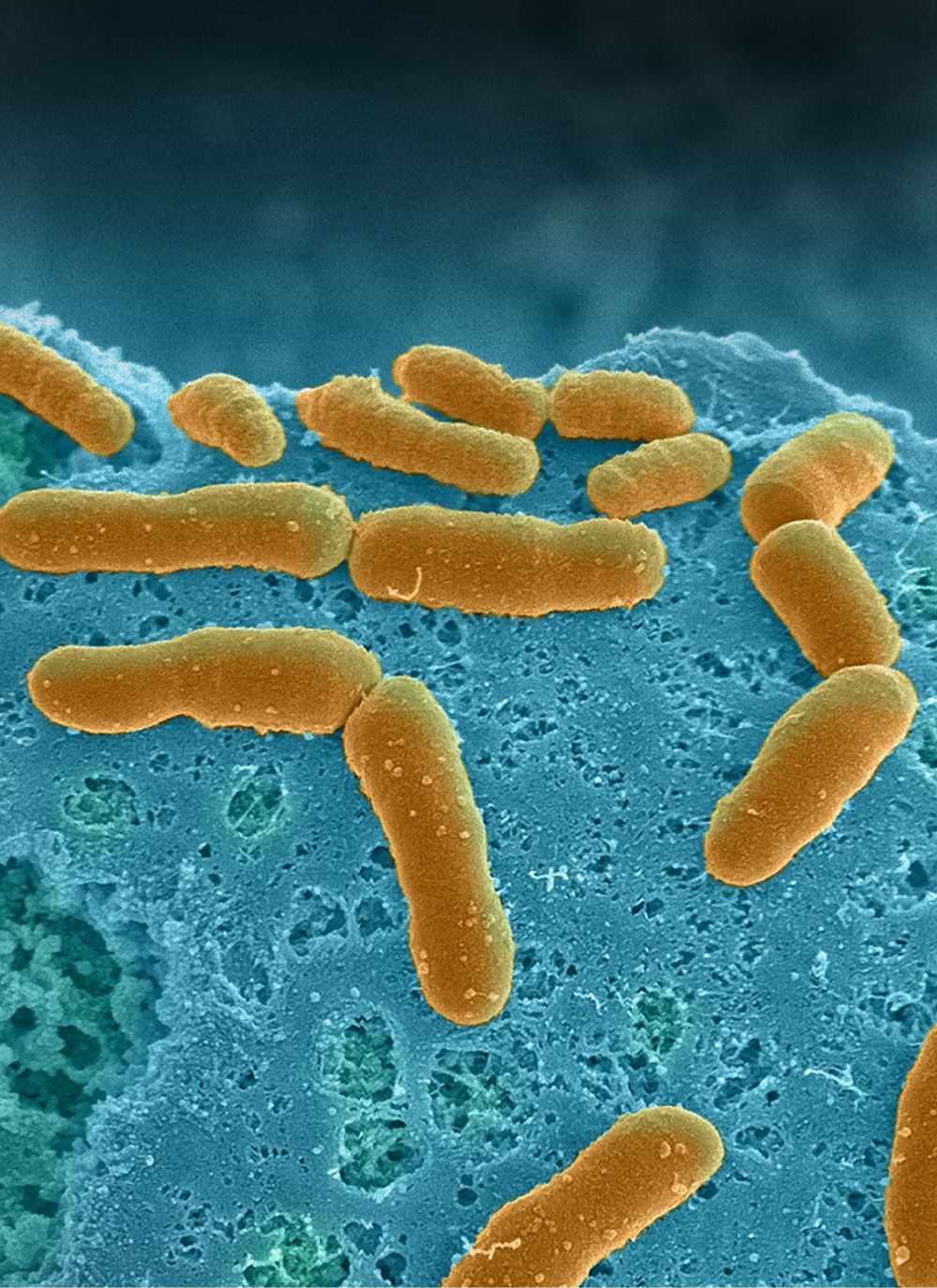
Viruses are masterful invaders. They cannibalize host cells by injecting their genetic material, often making thousands of copies of themselves in a single cell to ensure their replication and survival.
Some RNA viruses insert their genetic material as a single piece, while others chop it up into pieces. The latter are aptly named segmented viruses.
Such segmented RNA viruses—including several that cause human diseases like influenza—have been a longstanding enigma to researchers: How do they accomplish the precise copying and insertion of each segment? How do they ensure that individual segments are all copied by the same enzyme while ensuring that each segment can make different amounts of RNA? Such exquisite regulation is critical to make the correct levels of the viral proteins necessary for successful replication.