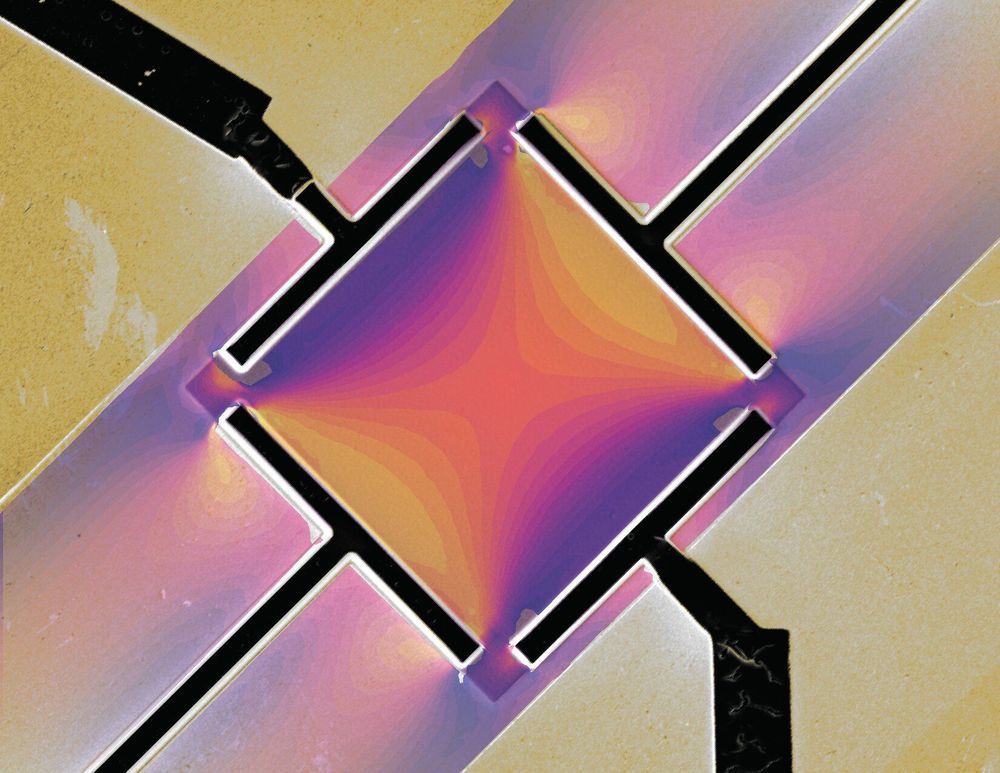
Researchers at EPFL have created a metallic microdevice in which they can define and tune patterns of superconductivity. Their discovery, which holds great promise for quantum technologies of the future, has just been published in Science.
In superconductors, electrons travel with no resistance. This phenomenon currently only occurs at very low temperatures. There are many practical applications, such as magnetic resonance imaging (MRI). Future technologies, however, will harness the total synchrony of electronic behavior in superconductors—a property called the phase. There is currently a race to build the world’s first quantum computer, which will use phases to perform calculations. Conventional superconductors are very robust and hard to influence, and the challenge is to find new materials in which the superconducting state can be easily manipulated in a device.
EPFL’s Laboratory of Quantum Materials (QMAT), headed by Philip Moll, has been working on a specific group of unconventional superconductors known as heavy fermion materials. The QMAT scientists, as part of a broad international collaboration between EPFL, the Max Planck Institute for Chemical Physics of Solids, the Los Alamos National Laboratory and Cornell University, made a surprising discovery about one of these materials, CeIrIn5.