I remember questioning this data, as it was not even research on animals, it was observation of people’s medical files.
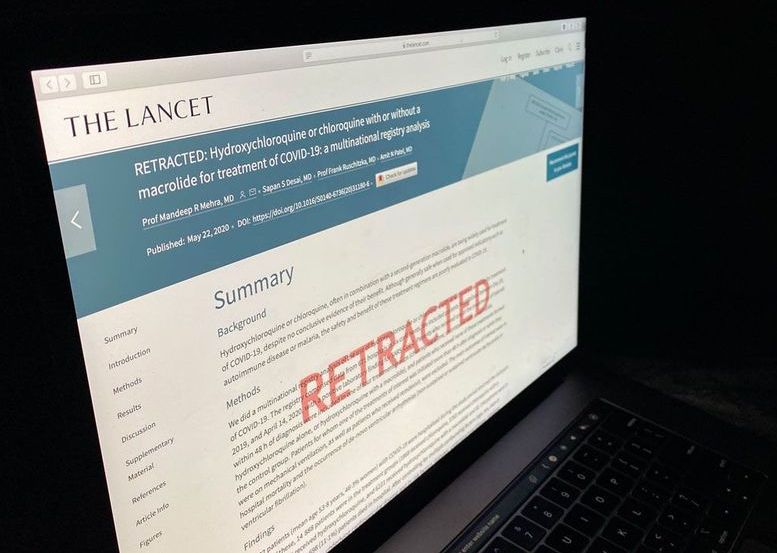
Three unlikely collaborators are at the heart of the fast-moving COVID-19 research scandal, which led to retractions last week by The Lancet and The New England Journal of Medicine (NEJM), and the withdrawal of an online preprint, after the trove of patient data they all relied on was challenged. The three physician-scientists never were at the same institution nor had they ever before written together, but they are the only authors in common on the disputed papers, and the other co-authors all have ties to at least one of them. Their partnership, which seized a high-impact role during a global public health crisis, has now ended disastrously.
The first author for both retracted papers was cardiac surgeon Mandeep Mehra, an eminent Harvard University professor who works at Brigham and Women’s Hospital (BWH) and is known internationally for cardiovascular medicine and heart transplants. He provided the kind of gravitas that can fast-track papers to leading journals. In a statement provided by BWH, Mehra said he had met another of the trio, cardiac surgeon Amit Patel, in “academic and medical circles,” and that Patel had introduced him to Sapan Desai, a vascular surgeon and founder of Surgisphere, the tiny company that supplied the data. Journal disclosures, however, also indicate Mehra received compensation from Triple-Gene, a gene therapy company Patel co-founded to develop cardiovascular treatments.
Author partnership on coronavirus papers is “completely bizarre” and should have been a red flag, former journal editor says.