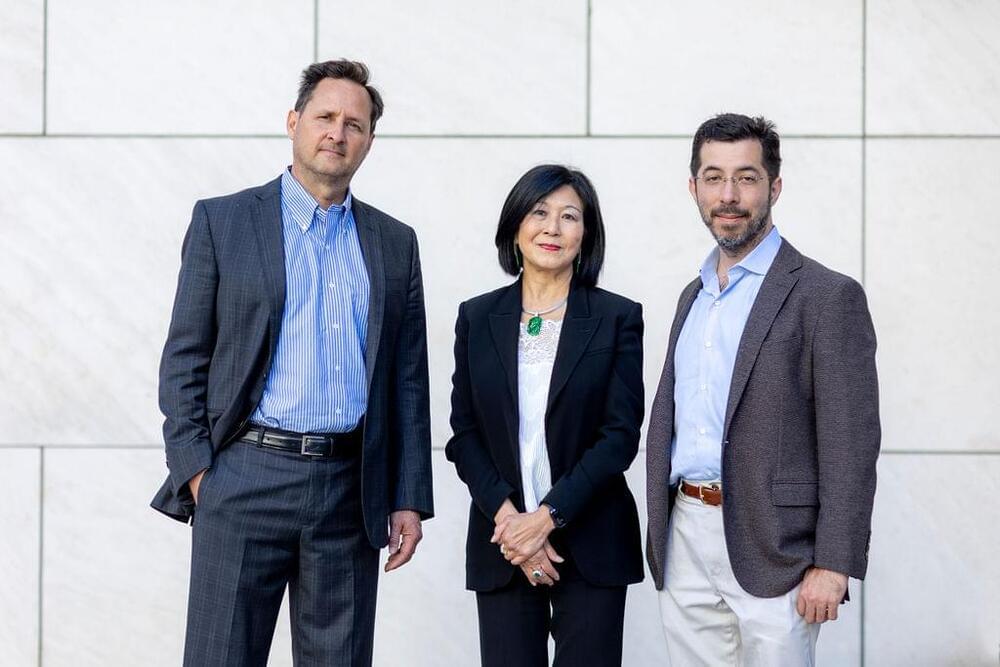
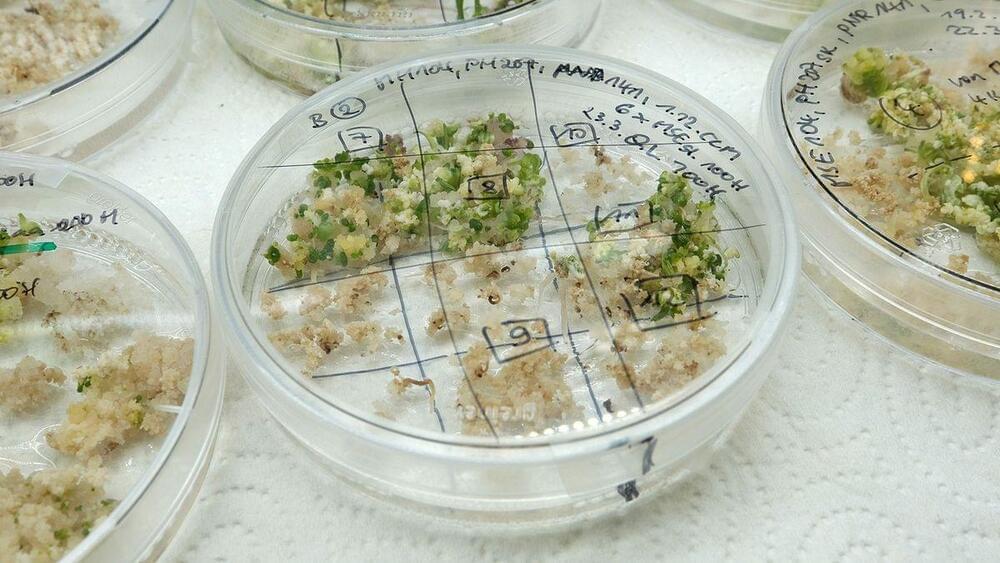
“We show that focusing on genes whose expression patterns are evolutionarily conserved across species enhances our ability to learn and predict ‘genes of importance’ to growth performance for staple crops, as well as disease outcomes in animals,” explained Gloria Coruzzi, Carroll & Milton Petrie Professor in NYU’s Department of Biology and Center for Genomics and Systems Biology and the paper’s senior author.
Machine learning can pinpoint “genes of importance” that help crops to grow with less fertilizer, according to a new study published in Nature Communications. It can also predict additional traits in plants and disease outcomes in animals, illustrating its applications beyond agriculture.
Using genomic data to predict outcomes in agriculture and medicine is both a promise and challenge for systems biology. Researchers have been working to determine how to best use the vast amount of genomic data available to predict how organisms respond to changes in nutrition, toxins, and pathogen exposure—which in turn would inform crop improvement, disease prognosis, epidemiology, and public health. However, accurately predicting such complex outcomes in agriculture and medicine from genome-scale information remains a significant challenge.
In the Nature Communications study, NYU researchers and collaborators in the U.S. and Taiwan tackled this challenge using machine learning, a type of artificial intelligence used to detect patterns in data.