Unlocking The Secrets Of Salamander Regeneration For Regenerative Therapies — Dr. Maximina Yun, Ph.D., CRTD / Center for Regenerative Therapies TU Dresden, Technische Universität Dresden.
Dr. Maximina Yun, Ph.D. (https://tu-dresden.de/cmcb/crtd/forschungsgruppen/crtd-forsc…oup-leader) is Research Group Leader at the Center for Regenerative Therapies Dresden (CRTD), Technical University Dresden, jointly affiliated with Max Planck Institute for Molecular Cell Biology and Genetics (MPI-CBG).
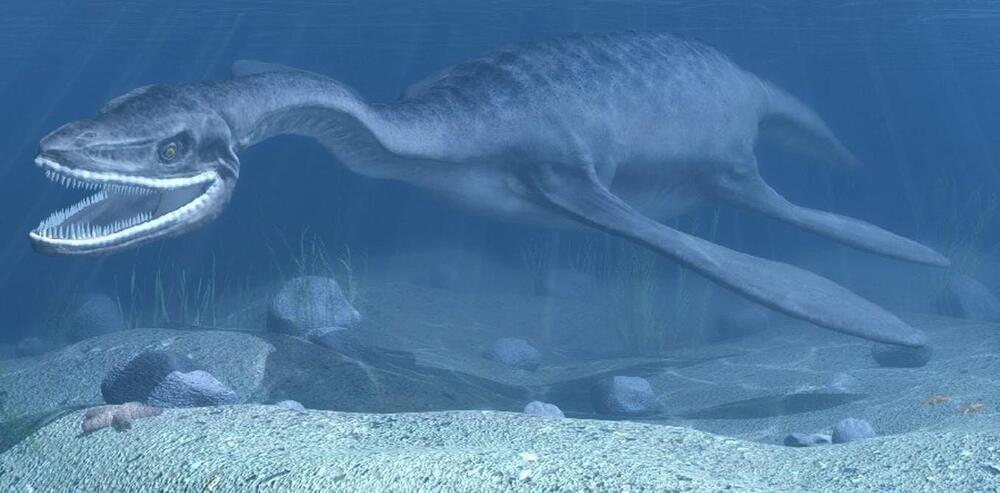
Dr. Yun and her group (https://tu-dresden.de/cmcb/crtd/forschungsgruppen/crtd-forschungsgruppen/yun) study the cellular and molecular basis of regeneration of complex structures with the help of salamanders (like newts and axolotls) and these vertebrates exceptional regenerative abilities, which in contrast to humans, are capable of regenerating complex tissues, and even entire organs, to a remarkable extent. Therefore, they offer unique insights into what molecular mechanisms must be in place for achieving quasi-perfect regeneration.
Research in the Yun group focuses on three main areas: describing cellular and molecular mechanisms driving regeneration (Mechanisms underlying the plasticity of the differentiated state), their connection with cellular aging (Role and regulation of senescence in regeneration), and the role that the immune system plays in regenerative context.
The research in the Yun group combines advanced molecular biology methods with state-of-the-art microscopy. Most recently the group has established Salamander-Eci, a novel method that enables the three-dimensional visualization of salamander tissues for a more comprehensive understanding of regenerative processes.