Results from the first phase 3 trial of using MDMA for PTSD along with talk therapy found the drug to be effective.
Glucose is the sugar we absorb from the foods we eat. It is the fuel that powers every cell in our bodies. Could glucose also power tomorrow’s medical implants?
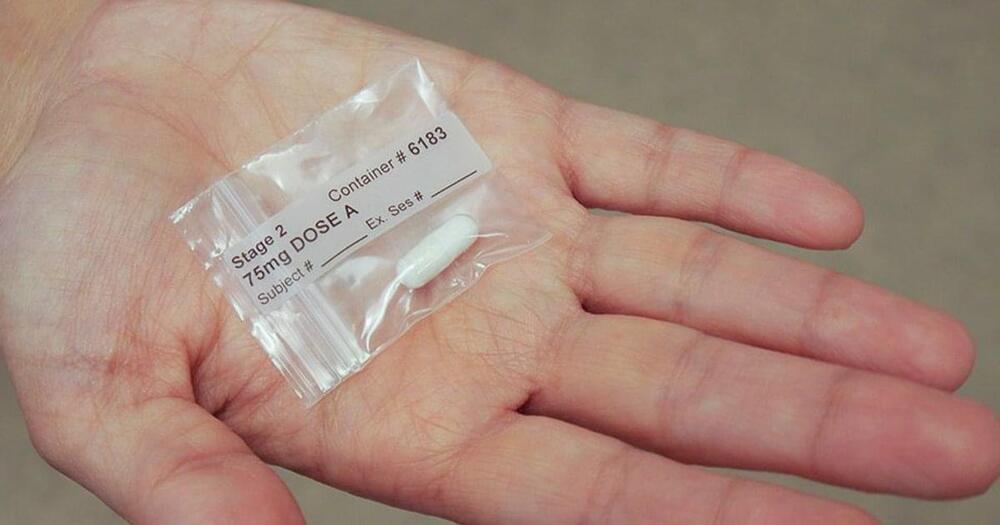
Engineers at MIT and the Technical University of Munich think so. They have designed a new kind of glucose fuel cell that converts glucose directly into electricity. The device is smaller than other proposed glucose fuel cells, measuring just 400 nanometers thick. The sugary power source generates about 43 microwatts per square centimeter of electricity, achieving the highest power density of any glucose fuel cell to date under ambient conditions.
Silicon chip with 30 individual glucose micro fuel cells, seen as small silver squares inside each gray rectangle. (Image: Kent Dayton)
Dr. Thomas Lehner was tired of his research repeatedly hitting a wall.
A scientist at the National Institute of Mental Health, Lehner studies the genetic underpinnings of neuropsychiatric disorders. Teasing out associated genes turned out to be relatively simple. Schizophrenia, for example, is linked to small variations in some 360 genes.
The problem is identifying the ones that really matter—culprit gene variants that can be turned into predictive tests, similar to the BRCA gene for breast cancer.
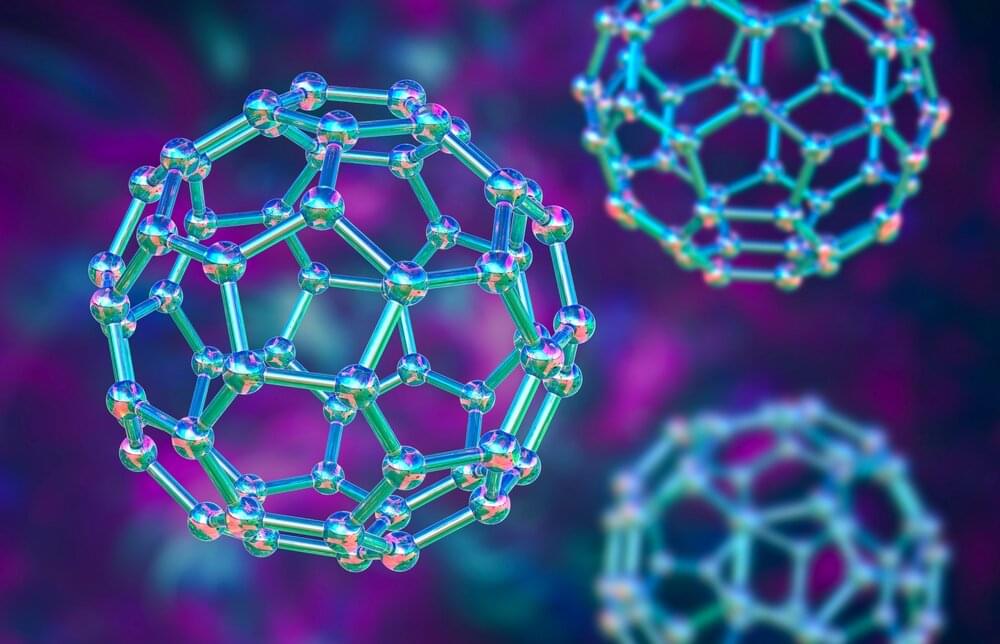
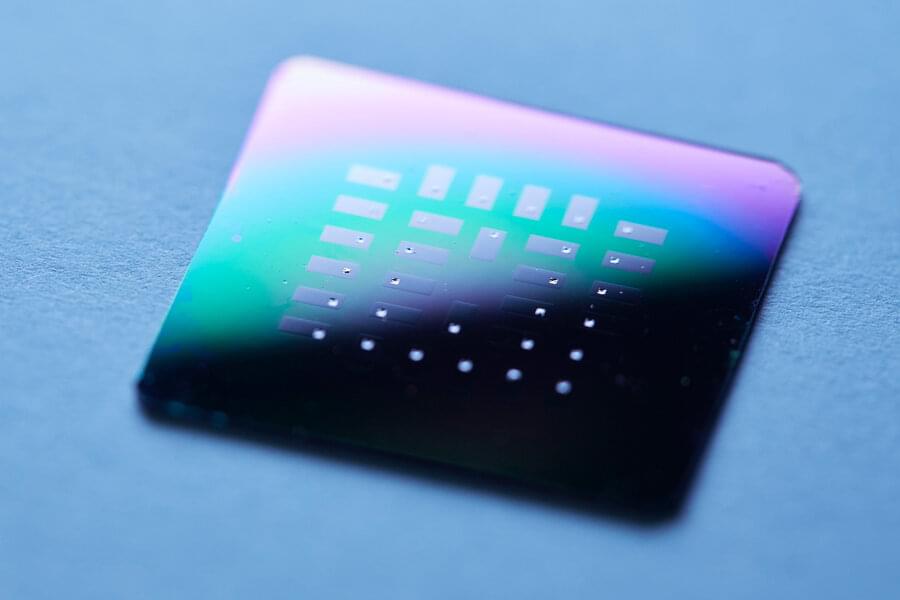
Russian scientists have synthesized a new ultra-hard material consisting of scandium containing carbon. It consists of polymerized fullerene molecules with scandium and carbon atoms inside. The work paves the way for future studies of fullerene-based ultra-hard materials, making them a potential candidate for photovoltaic and optical devices, elements of nanoelectronics and optoelectronics, and biomedical engineering as high-performance contrast agents. The study was published in Carbon.
The discovery of new, all-carbon molecules known as fullerenes almost 40 years ago was a revolutionary breakthrough that paved the way for fullerene nanotechnology. Fullerenes have a spherical shape made of pentagons and hexagons that resembles a soccer ball, and a cavity within the carbon frame of fullerene molecules can accommodate a variety of atoms.
The introduction of metal atoms into carbon cages leads to the formation of endohedral metallofullerenes (EMF), which are technologically and scientifically important owing to their unique structures and optoelectronic properties.


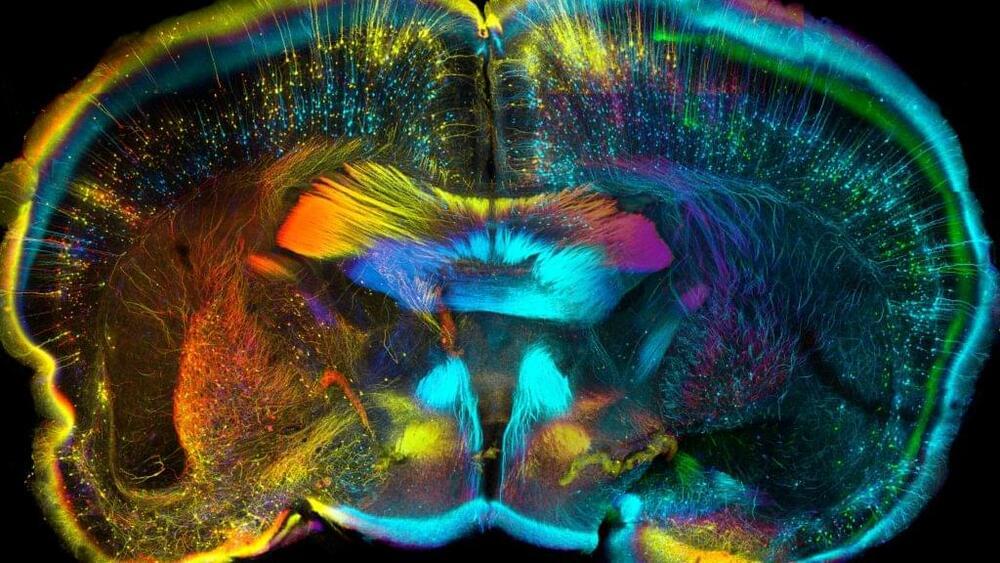
For a human, one of the first signs someone is getting old is the inability to remember little things; maybe they misplace their keys, or get lost on an oft-taken route. For a laboratory mouse, it’s forgetting that when bright lights and a high-pitched buzz flood your cage, an electric zap to the foot quickly follows.
But researchers at Stanford University discovered that if you transfuse cerebrospinal fluid from a young mouse into an old one, it will recover its former powers of recall and freeze in anticipation. They also identified a protein in that cerebrospinal fluid, or CSF, that penetrates into the hippocampus, where it drives improvements in memory.
The tantalizing breakthrough, published Wednesday in Nature, suggests that youthful factors circulating in the CSF, or drugs that target the same pathways, might be tapped to slow the cognitive declines of old age. Perhaps even more importantly, it shows for the first time the potential of CSF as a vehicle to get therapeutics for neurological diseases into the hard-to-reach fissures of the human brain.
