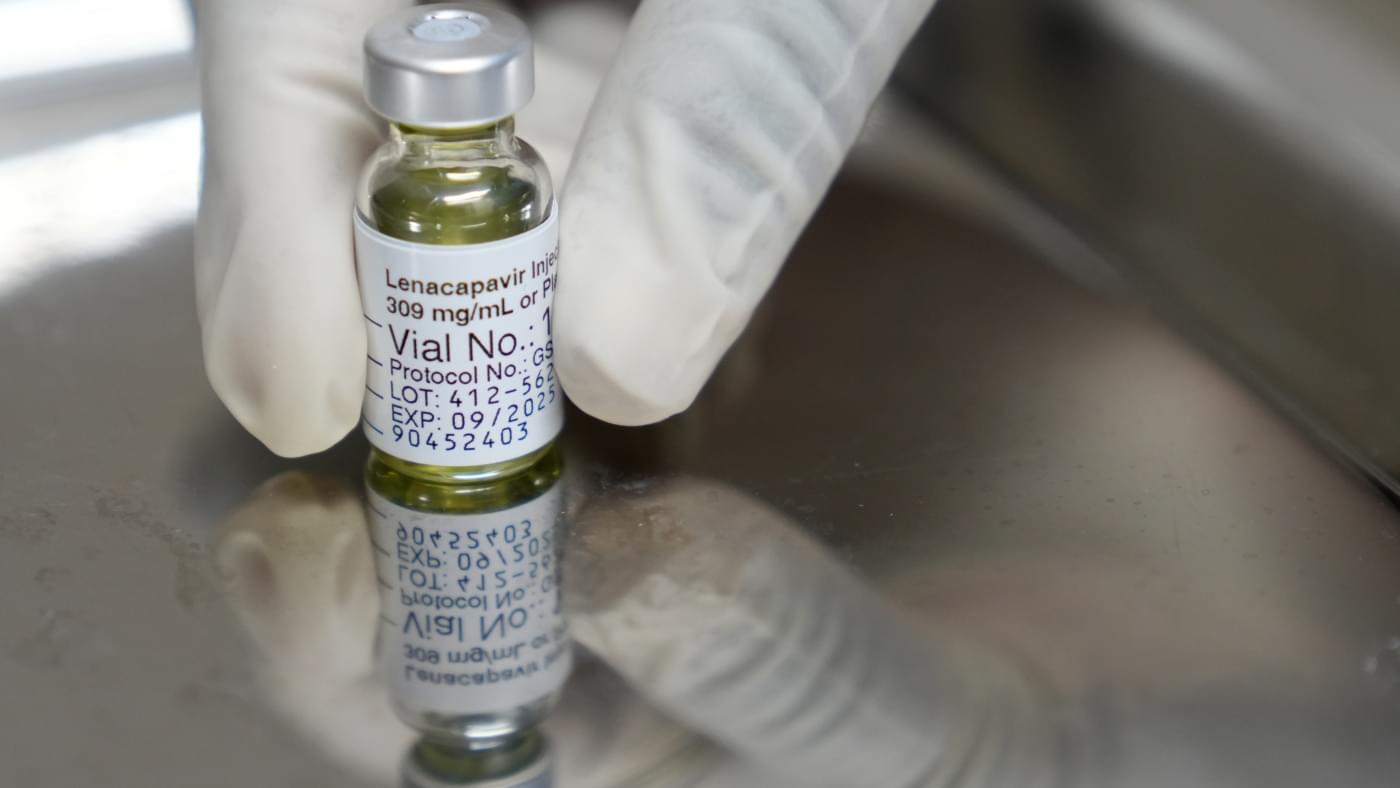
A drug called lenacapavir, administered in two injections a year, offers protection from HIV comparable to daily pills. One looming question: Will it be affordable for lower resource countries?

Insulin resistance detected by routine triglyceride-glucose (TyG) index can flag people with early Alzheimer’s who are four times more likely to present rapid cognitive decline, according to new research presented at the European Academy of Neurology (EAN) Congress 2025.
Neurologists at the University of Brescia reviewed records of 315 non-diabetic patients with cognitive deficits, including 200 with biologically confirmed Alzheimer’s disease. All subjects underwent an assessment of insulin resistance using the TyG index and a clinical follow-up of three years.
The work is published in the journal Alzheimer’s & Dementia.
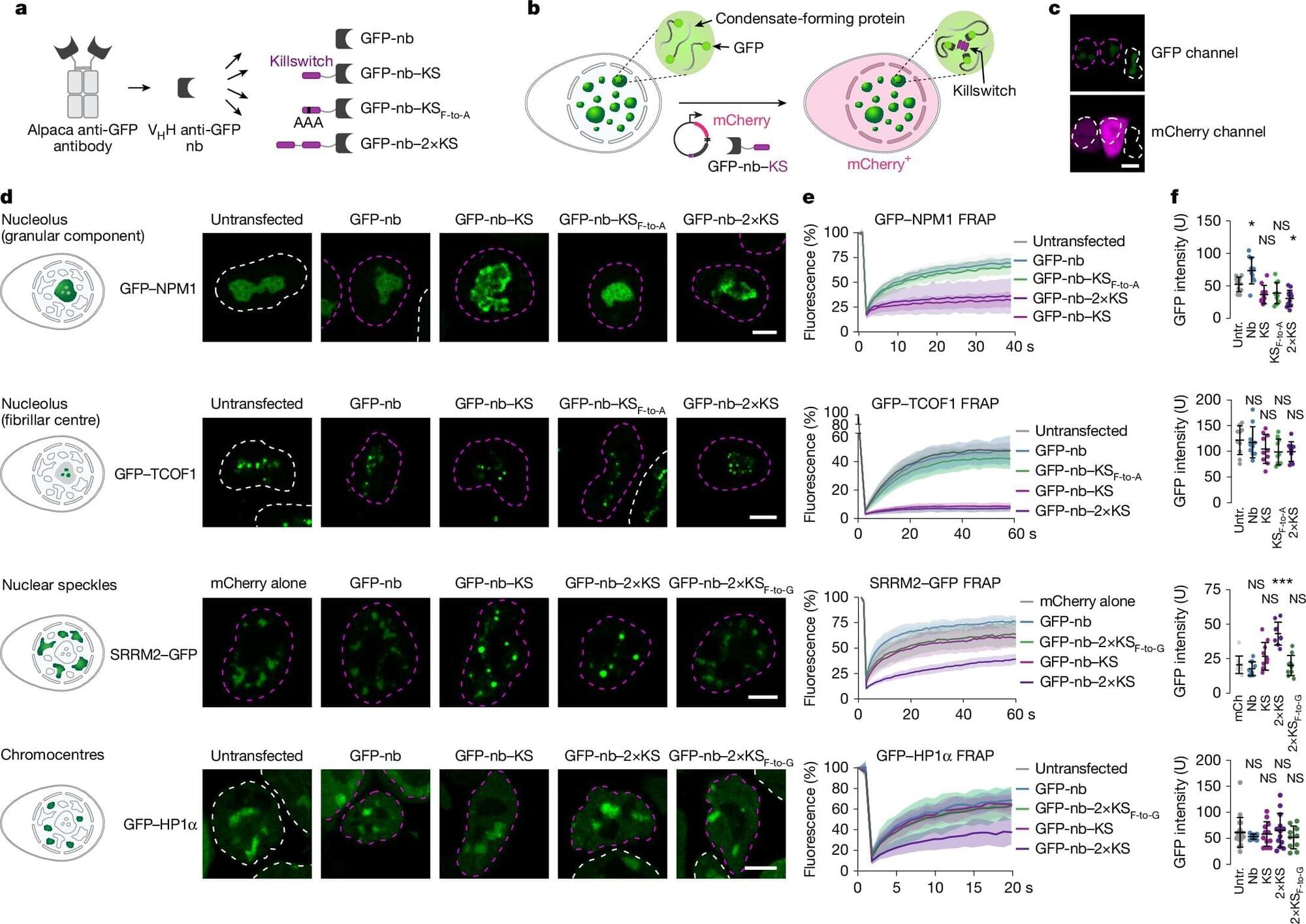
Researchers at the Max Planck Institute for Molecular Genetics have developed a novel synthetic micropeptide termed the “killswitch” to selectively immobilize proteins within cellular condensates, unveiling crucial connections between condensate microenvironments and their biological functions.
Biomolecular condensates are specialized regions inside cells, existing without membranes, where critical biochemical reactions occur. Their importance in health and disease is well established, including roles in cancer progression and viral infection.
Methods to precisely probe and manipulate condensates in living cells remain limited. Existing strategies lack specificity, either dissolving condensates indiscriminately or requiring artificial protein overexpression, which obscures the natural behavior of native cellular proteins.
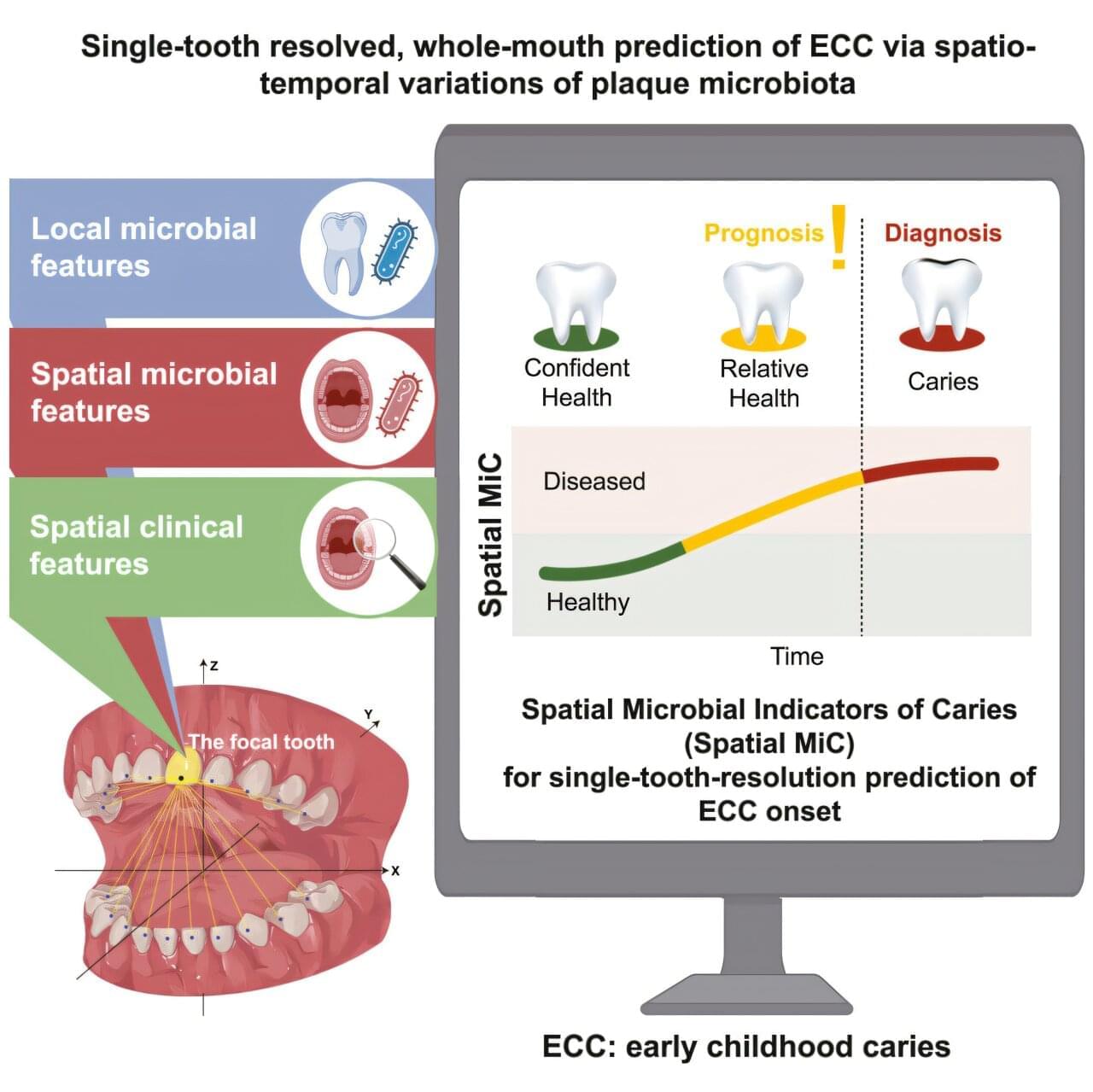
Early childhood caries (ECC)—the world’s most prevalent chronic childhood disease—disproportionately targets specific teeth, a mystery that has remained unresolved until now.
A collaborative research team from the Faculty of Dentistry of the University of Hong Kong (HKU), Chinese Academy of Sciences (CAS-QIBEBT), Qingdao Stomatological Hospital, and Qingdao Women and Children’s Hospital has made a discovery that could revolutionize the prevention of childhood tooth decay.
The team has developed the world’s first artificial intelligence (AI) system capable of predicting early childhood caries risk for individual teeth based on microbial characteristics, achieving an accuracy rate of more than 90%. The study is published in Cell Host & Microbe.
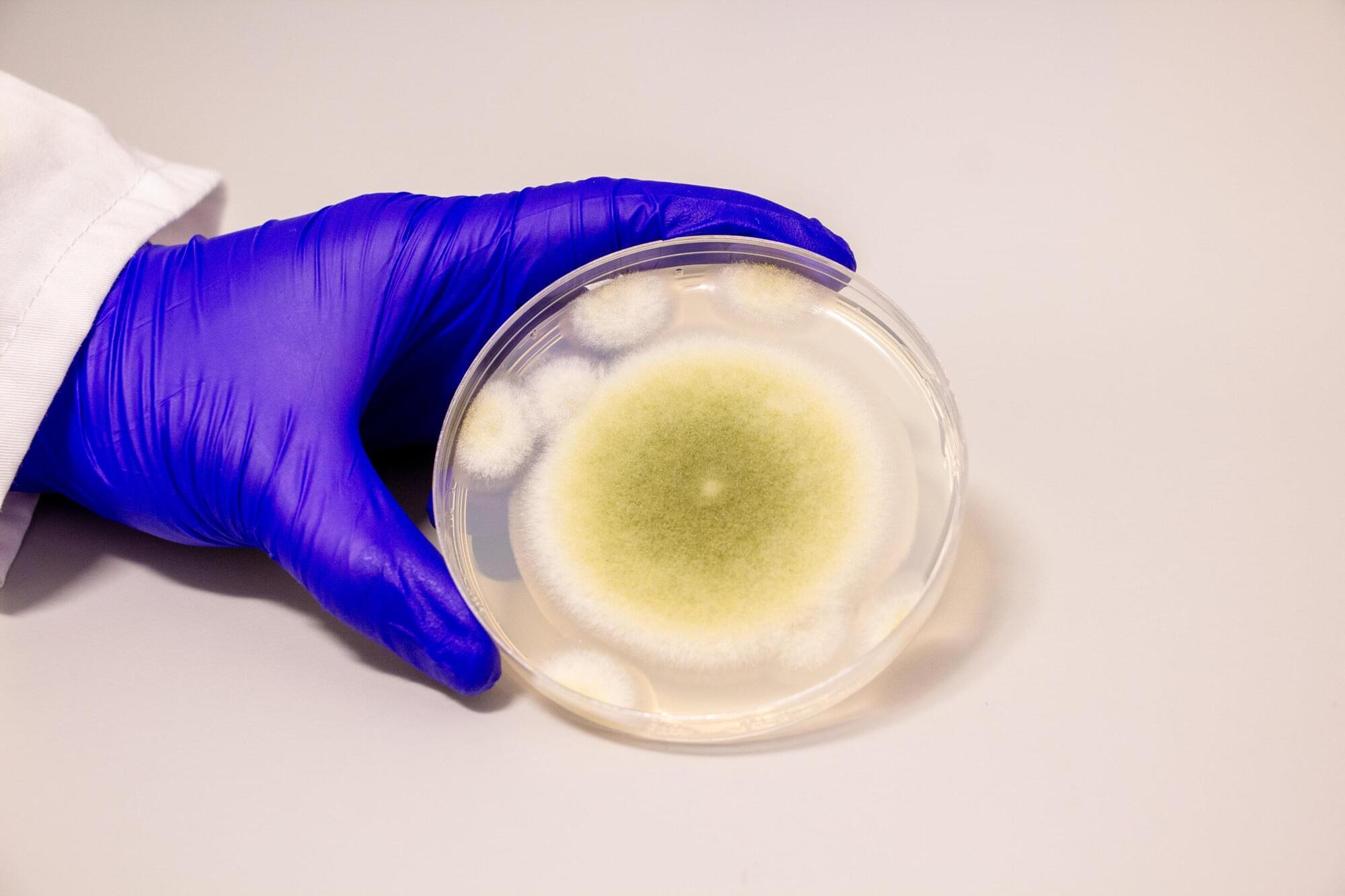
Penn-led researchers have turned a deadly fungus into a potent cancer-fighting compound. After isolating a new class of molecules from Aspergillus flavus, a toxic crop fungus linked to deaths in the excavations of ancient tombs, the researchers modified the chemicals and tested them against leukemia cells. The result? A promising cancer-killing compound that rivals FDA-approved drugs and opens up new frontiers in the discovery of more fungal medicines.
“Fungi gave us penicillin,” says Sherry Gao, Presidential Penn Compact Associate Professor in Chemical and Biomolecular Engineering (CBE) and in Bioengineering (BE) and senior author of a new paper in Nature Chemical Biology on the findings. “These results show that many more medicines derived from natural products remain to be found.”

Most treatments for Parkinson’s disease (PD) only slow disease progression. Early intervention for the neurological disease that worsens over time is therefore critical to optimize care, but that requires early diagnosis. Current tests, like clinical rating scales and neural imaging, can be subjective and costly. Now, researchers in ACS’ Analytical Chemistry report the initial development of a system that inexpensively screens for PD from the odors in a person’s earwax.
Previous research has shown that changes in sebum, an oily substance secreted by the skin, could help identify people with PD. Specifically, sebum from people with PD may have a characteristic smell because volatile organic compounds (VOCs) released by sebum are altered by disease progression — including neurodegeneration, systemic inflammation and oxidative stress.
However, when sebum on the skin is exposed to environmental factors like air pollution and humidity, its composition can be altered, making it an unreliable testing medium. But the skin inside the ear canal is kept away from the elements. So, Hao Dong, Danhua Zhu and colleagues wanted to focus their PD screening efforts on earwax, which mostly consists of sebum and is easily sampled.
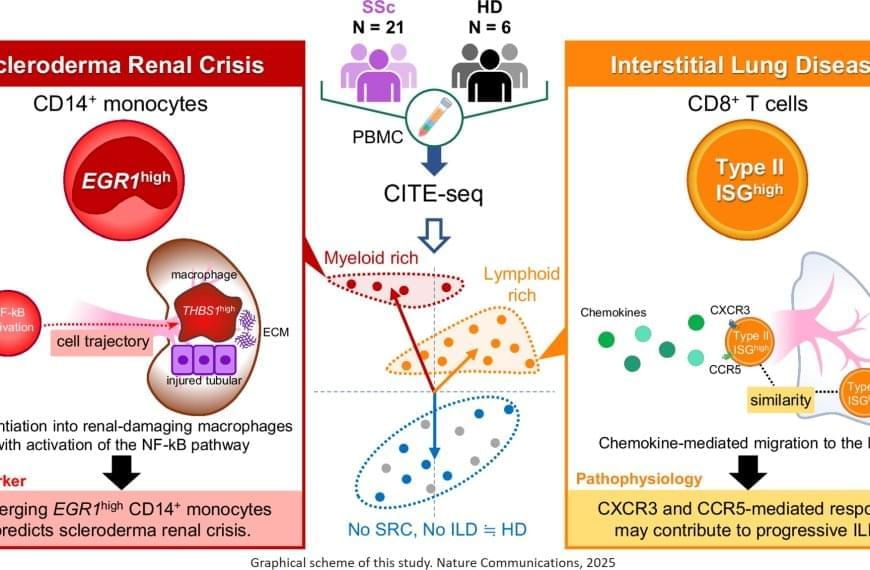
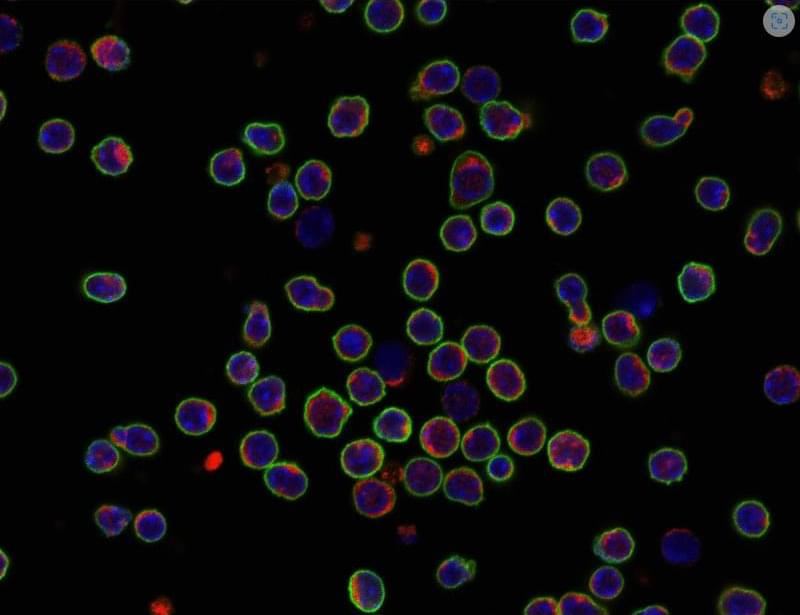
“We know that immune dysregulation causes vascular damage and tissue fibrosis in systemic sclerosis,” says the lead author. “However, it remains unclear why skin symptoms and the level of organ involvement differ from patient to patient.”
To explore this, the researchers took blood and tissue samples from patients with systemic sclerosis and analyzed them cell by cell, looking for differences in gene expression. Additionally, proteins on the cell surface were examined to identify biomarkers of disease, which are useful for identifying and treating diseases in earlier stages.
“The results were intriguing,” explains the senior author. “We identified a specific subset of immune cells, the EGR1-expressing subpopulation of CD14+ monocytes, that were clearly associated with scleroderma renal crisis, a serious kidney complication in patients with systemic sclerosis.”
While immune cells usually help the body fight infection and disease, in certain cases they can be inappropriately activated through gene expression. In this instance, CD14+ monocytes differentiated – or transformed – into destructive macrophages, which can further promote inflammation near the kidneys and contribute to the thickening and scarring of internal organs.
In addition, the researchers found that CD8+ T cells with a type II interferon signature, which makes the immune cells particularly aggressive and inflammatory, were linked to progressive interstitial lung disease. EGR1-expressing CD14+ monocytes and these peculiar CD8+ T cells are likely to accumulate in the kidney or the lung, respectively, and produce or recruit other factors that contribute to disease progression.
Treating rare diseases can be complicated at the best of times, and it gets even more complicated when different patients with the same disease exhibit different symptoms. Now, researchers have reported a cellular signature that might explain why some patients with autoimmune disease are stable while others face life-threatening complications.