The tool can identify symptoms of dengue, malaria, leptospirosis, and scrub typhus.
The study investigates both statistical and machine learning approaches. WHO has categorized dengue as a “neglected tropical disease.”
A prediction tool based on multi-nominal regression analysis and a machine learning algorithm was developed.
Accurate diagnosis is essential for the proper treatment and ensuring the well-being of patients. However, some diseases present with similar clinical symptoms and laboratory results, making diagnosing them more challenging.
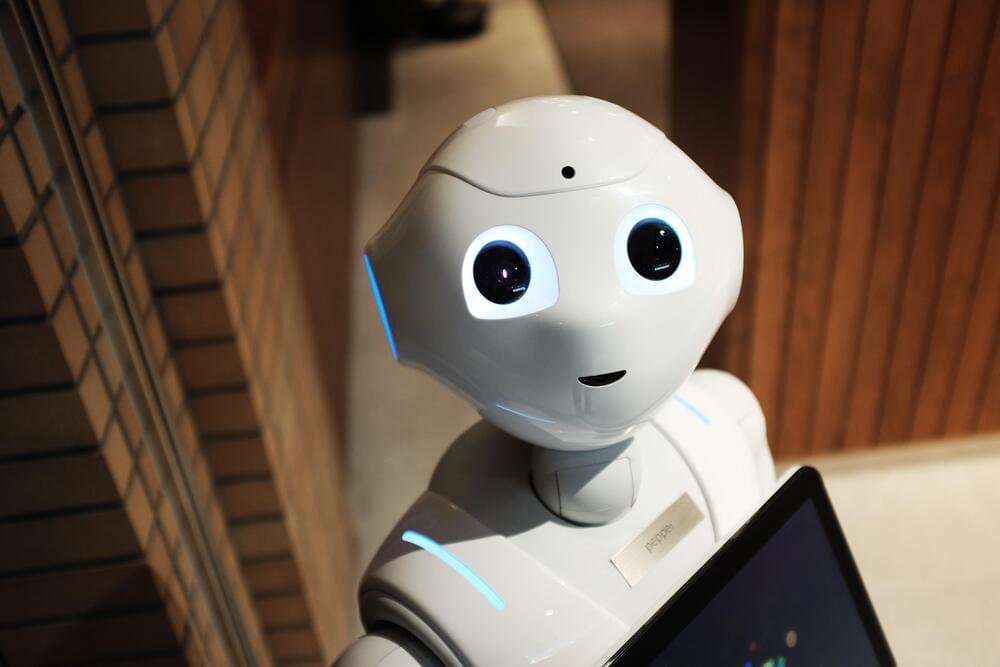
Artificial Intelligence is perhaps the most promising technology for transforming our lives — but it’s also incredibly scary. At CES 2022, A panel of AI experts discussed what role AI might play in the future of healthcare.
In a session titled “Consumer Safety Driven by AI,” Pat Baird, an AI engineer and software developer who works in standards and regulations for Phillips, and Joseph Murphy, VP Marketing at Sensory Inc., an American technology company that develops AI products, discussed what AI could add to our lives. They also discussed the apprehension many people feel about the technology.