Despite their names, artificial intelligence technologies and their component systems, such as artificial neural networks, don’t have much to do with real brain science. I’m a professor of bioengineering and neurosciences interested in understanding how the brain works as a system – and how we can use that knowledge to design and engineer new machine learning models.
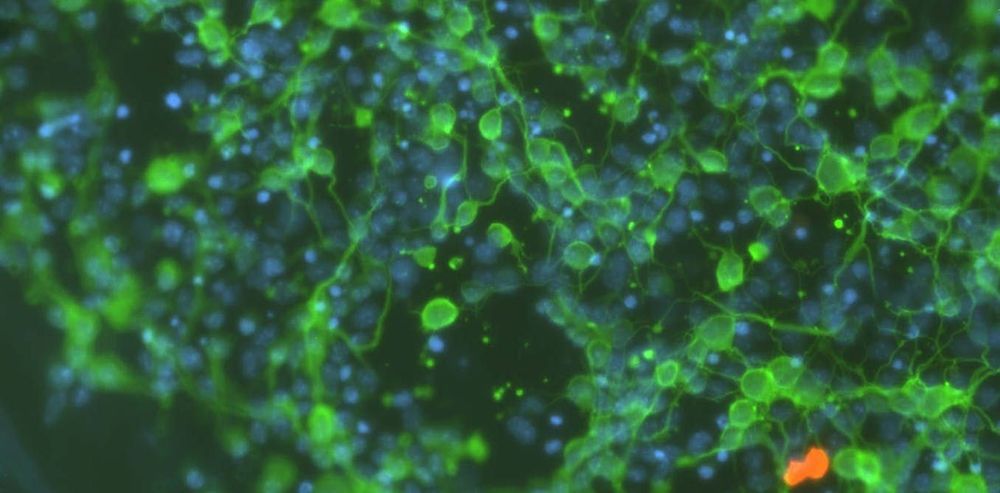
In recent decades, brain researchers have learned a huge amount about the physical connections in the brain and about how the nervous system routes information and processes it. But there is still a vast amount yet to be discovered.
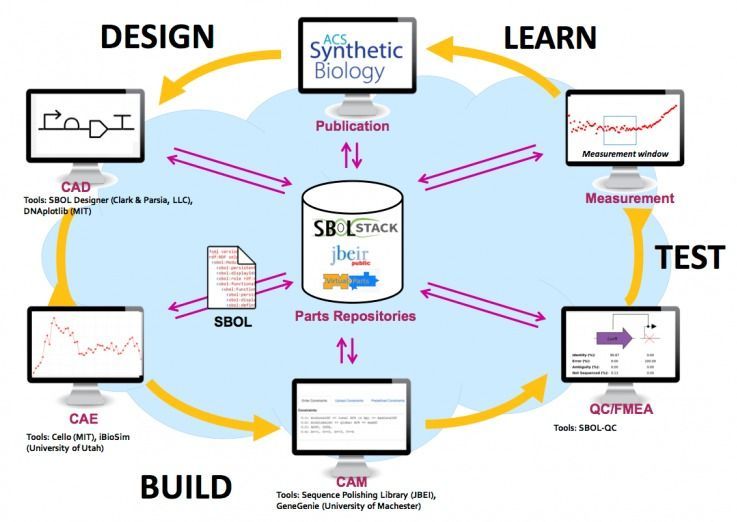
At the same time, computer algorithms, software and hardware advances have brought machine learning to previously unimagined levels of achievement. I and other researchers in the field, including a number of its leaders, have a growing sense that finding out more about how the brain processes information could help programmers translate the concepts of thinking from the wet and squishy world of biology into all-new forms of machine learning in the digital world.