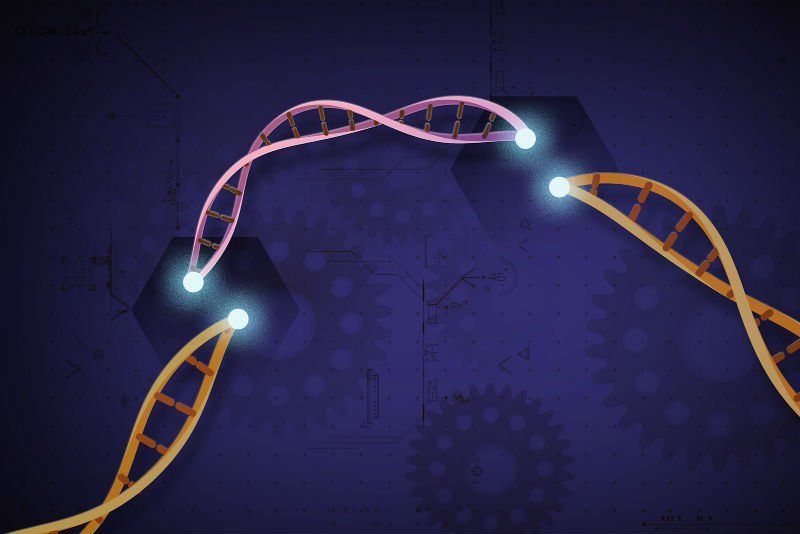
The evolving gene-editing technology CRISPR-Cas9 is useful for changing one gene, or maybe a few genes at a time. A team at ETH Zurich has tweaked the technology so they can change 25 different gene sites at once. Instead of using the Cas9 enzyme to do the DNA cutting, though, they used Cas12a. That allowed them to create a long “address list” of gene sites to target, they explained in the journal Nature Methods. They created a DNA molecule called a plasmid to store the list, inserted it in human cells and were able to modify several genes, they reported. (Release)
Chemotherapy and radiation suppress blood stem cells, often for several weeks or even months after cancer treatments are complete. This leaves patients vulnerable to infections and other health problems. Scientists at the University of California, Los Angeles have created a new drug that targets the protein tyrosine phosphatase-sigma (PTP-sigma), which is prevalent on blood stem cells. They showed that blocking the protein in rodent models with the drug, called DJ009, helped blood cells recover more quickly after they were damaged by radiation. They published their findings in the journal Nature Communications. (Release)