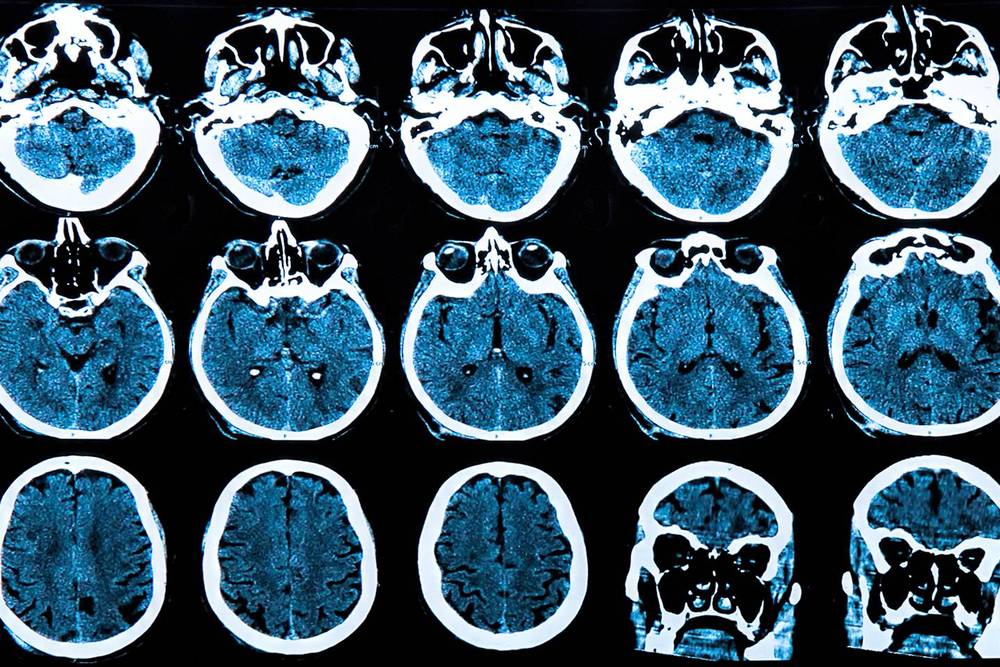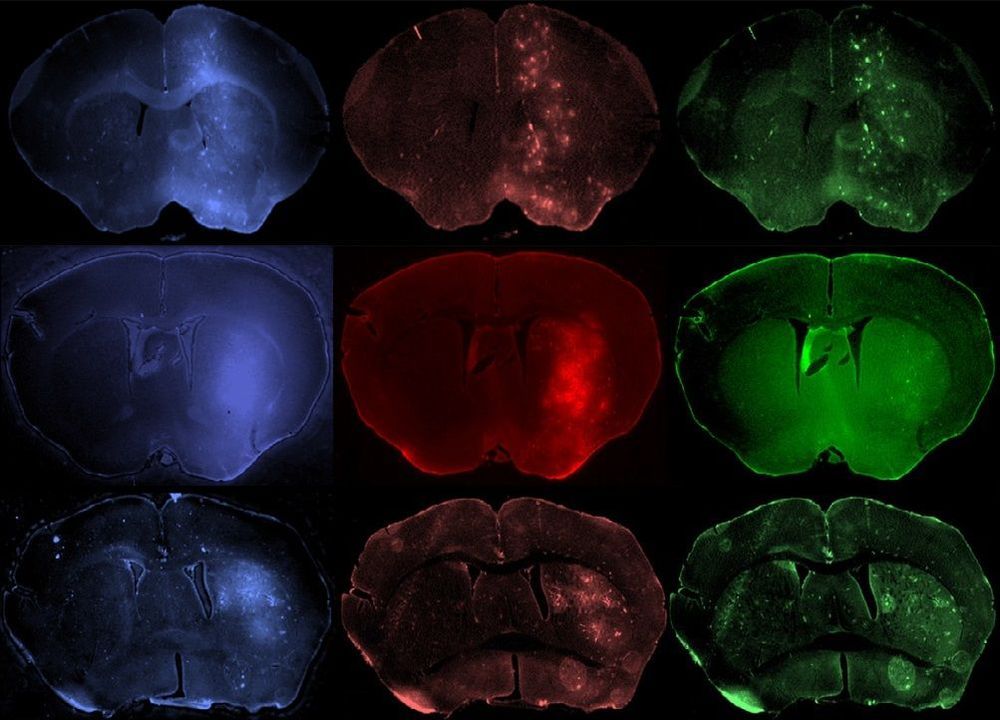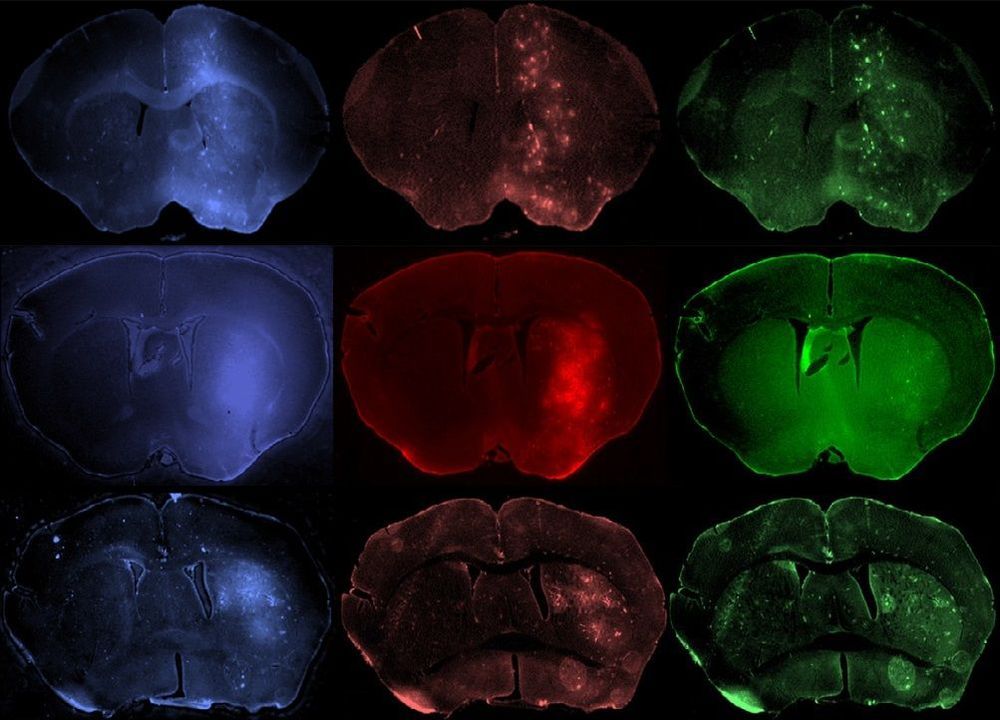
Focused ultrasound (FUS) can be used to help drugs pass from the bloodstream into the brain, but the technique’s effectiveness depends on the ultrasound pressure and the size of the drug molecules. Michael Valdez and colleagues at the University of Arizona measured how thoroughly differently sized molecules diffused into mouse brains under a range of ultrasound intensities, and found that the largest molecules could not be delivered under any safe FUS regime. The results set a limit on the types of drugs that might one day be used to treat neurological conditions like Alzheimer’s and Parkinson’s disease (Ultrasound Med. Biol. 10.1016/j.ultrasmedbio.2019.08.024).
Usually, the brain is isolated from substances circulating in the bloodstream by the blood–brain barrier (BBB), a semipermeable layer of cells that permits only certain molecules to pass. This restricts the range of drugs that can be used in the brain to small, hydrophobic molecules (such as alcohol and caffeine), other small drugs like psychotropics and some antibiotics. Extending that range would open the door to new therapeutic possibilities, says Theodore Trouard, who led the team. “The ability to temporarily and safely open the BBB to allow drugs into the brain would help address a number of neurological diseases for which there is currently no effective treatment.”
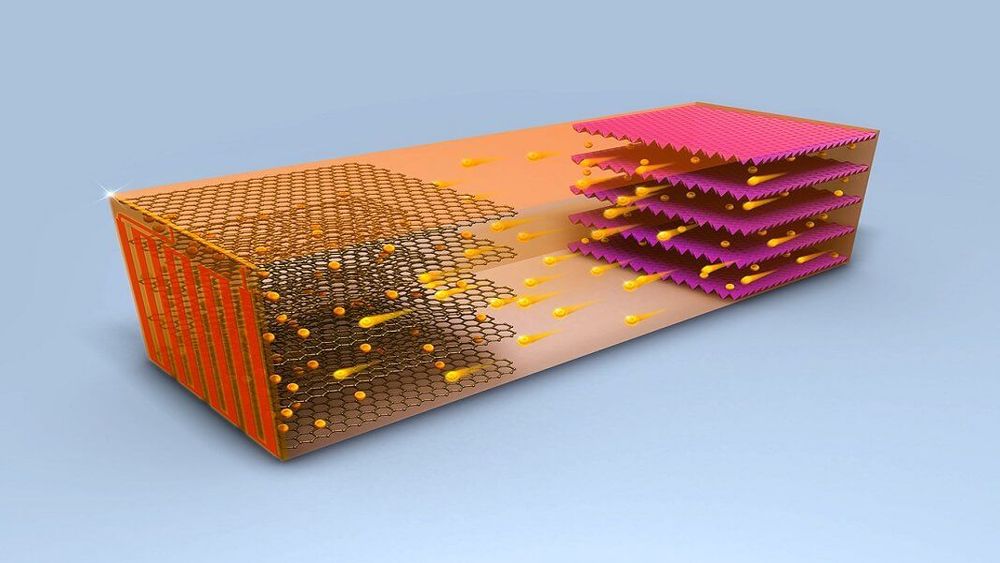
Previous research has shown that such opening can be achieved by focusing an ultrasound beam in the brain while gas microbubbles circulate in the blood. The microbubbles – perfluorocarbon-filled lipid shells about 1 µm across – are inert while they move around the body, but rapidly expand and contract in the local pressure fluctuations caused by the ultrasound field. Mechanical forces exerted by this phenomenon create temporary gaps in the layer of cells that make up the BBB, giving larger molecules a chance to breach the brain’s defences.