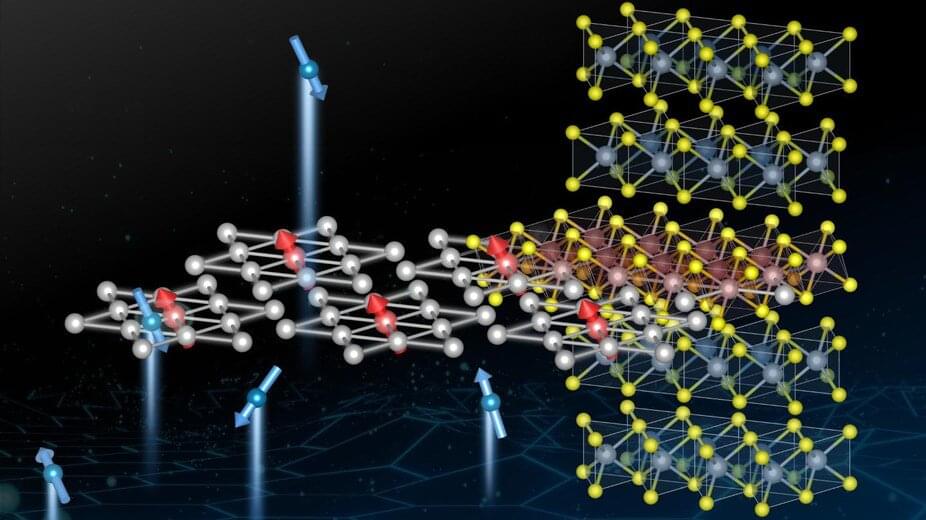
An international team led by EPFL scientists, has unveiledthat has only been observed in engineered atomic thin layers. The phenomenon can be reproduced by the native defects of lab grown large crystals, making future investigation of Kondo systems and quantum electronic devices more accessible.
The properties of materials that are technologically interesting often originate from defects on their atomic structure. For example, changing the optical properties of rubies with chrome inclusions has helped develop lasers, while nitrogen-vacancy in diamonds are paving the way for applications such as quantum magnetometers. Even in the metallurgical industry, atomic-scale defects like dislocation enhances the strength of forged steel.
Another manifestation of atomic-scale defects is the Kondo effect, which affects a metal’s conduction properties by scattering and slowing the electrons and changing the flow of electrical current through it. This Kondo effect was first observed in metals with very few magnetic defects, e.g. gold with few parts per million of iron inclusions. When the diluted magnetic atoms align all the electrons spin around them, this slows the electrical current motion inside the material, equally along every direction.