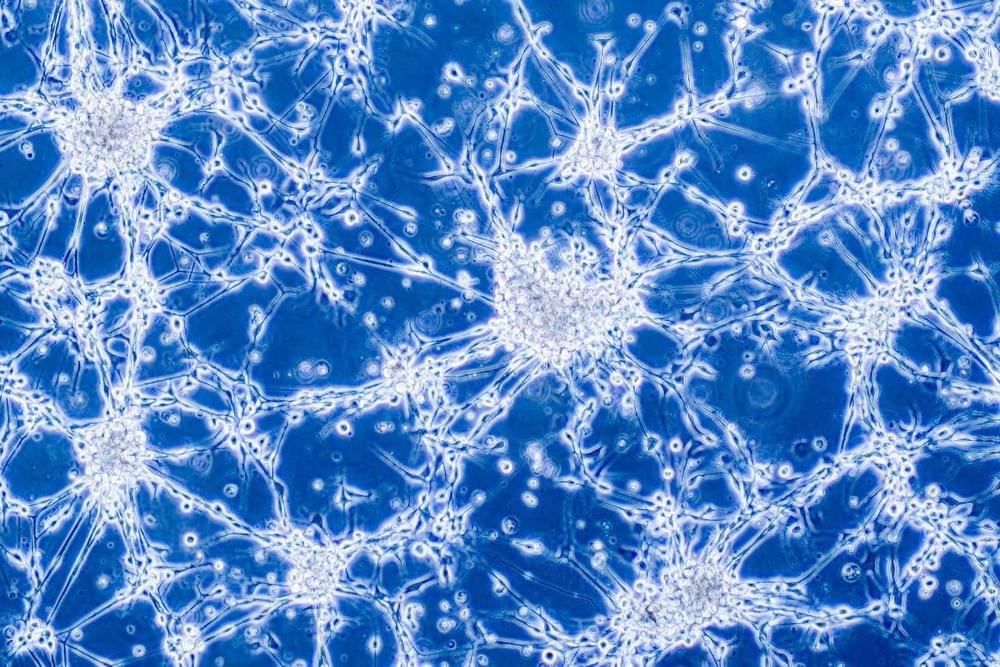
Are quantum events required for consciousness in a very special sense, far beyond the general sense that quantum events are part of all physical systems? What would it take for quantum events, on such a micro-scale, to be relevant for brain function, which operates at the much higher level of neurons and brain circuits? What would it mean?
Free access to Closer to Truth’s library of 5,000 videos: http://bit.ly/376lkKN
Watch more interviews on the Quantum Physics of Consciousness: https://bit.ly/37xFvYm.
Menas Kafatos is a physicist and the Director of the Center of Excellence and has served as Founding Dean, Schmid College of Science & Technology at Chapman University.
Register for free at CTT.com for subscriber-only exclusives: http://bit.ly/2GXmFsP
Closer to Truth, hosted by Robert Lawrence Kuhn and directed by Peter Getzels, presents the world’s greatest thinkers exploring humanity’s deepest questions. Discover fundamental issues of existence. Engage new and diverse ways of thinking. Appreciate intense debates. Share your own opinions. Seek your own answers.