Get the latest international news and world events from around the world.





Tesla’s 4680 battery cell pilot production line hits 70–80% yield: report
Tesla has a number of programs that have the potential to change markets, and one of these is arguably the 4,680 cells. Created using a dry electrode process and optimized for price and efficiency, the 4,680 batteries could very well be the key to Tesla’s possible invasion of the mainstream auto and energy market. If Tesla pulls off its 4,680 production ramp, its place at the summit of the sustainable energy market would be all but ensured.
Unfortunately, Tesla’s publicly disclosed target for the 4,680 cells’ production ramp appears to have been made on “Elon Time.” This means that during Battery Day last year, Tesla’s target of hitting a capacity of 10 GWh by late September2021included some optimistic assumptions. Similar to other projects like Elon Musk’s Alien Dreadnaught factory, however, the pilot production of the 4,680 cells have met some challenges.
Tesla admitted to these difficulties during the Q22021earnings call, when Elon Musk explained that one of the main challenges in the 4,680 cell production ramp was related to the batteries’ calendaring, or the process when the dry cathode material is squashed to a particular height. Partly due to the use of nickel in the 4,680 cells, which are extremely hard, some of the calendar rolls end up being dented.
The World’s Biggest Wind Turbine Is Being Built in China
The turbine will be taller than the GE building in New York’s Rockefeller Center, and each of its blades longer than an American football field.

New observations challenge popular radio burst model
Strange behavior caught by two radio observatories may send theorists back to the drawing board.
Fourteen years ago, the first fast radio burst (FRB) was discovered. By now, many hundreds of these energetic, millisecond-duration bursts from deep space have been detected (most of them by the CHIME radio observatory in British Columbia, Canada), but astronomers still struggle to explain their enigmatic properties. A new publication in this week’s Nature “adds a new piece to the puzzle,” says Victoria Kaspi (McGill University, Canada). “In this field of research, surprising twists are almost as common as new results.”
Most astronomers agree that FRBs are probably explosions on the surfaces of highly magnetized neutron stars (so-called magnetars). But it’s unclear why most FRBs appear to be one-off events, while others flare repeatedly. In some cases, these repeating bursts show signs of periodicity, and scientists had come up with an attractive model to explain this behavior, involving stellar winds in binary systems.
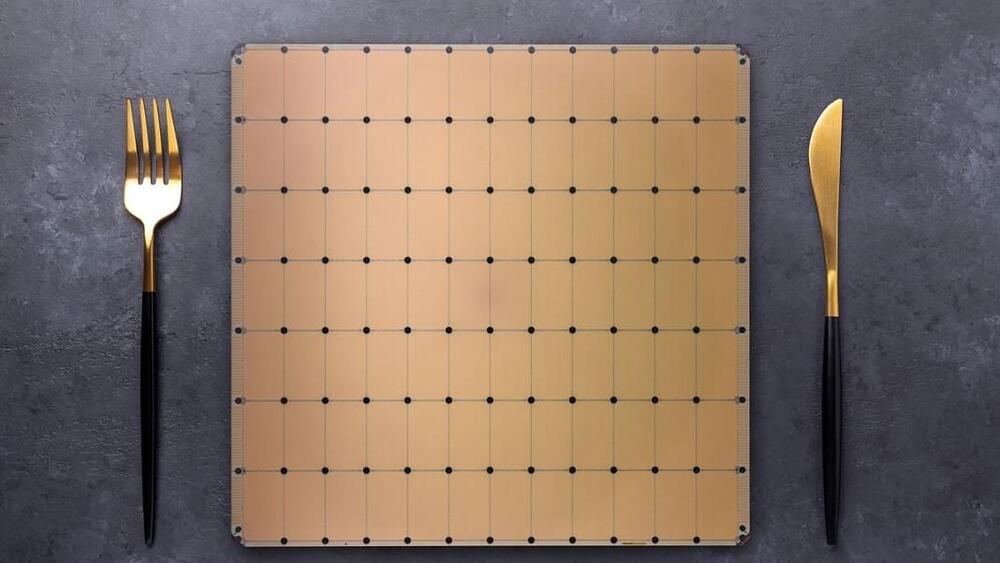
Cerebras Upgrades Trillion-Transistor Chip to Train ‘Brain-Scale’ AI
Much of the recent progress in AI has come from building ever-larger neural networks. A new chip powerful enough to handle “brain-scale” models could turbo-charge this approach.
Chip startup Cerebras leaped into the limelight in2019when it came out of stealth to reveal a 1.2-trillion-transistor chip. The size of a dinner plate, the chip is called the Wafer Scale Engine and was the world’s largest computer chip. Earlier this year Cerebras unveiled the Wafer Scale Engine 2 (WSE-2), which more than doubled the number of transistors to 2.6 trillion.
Now the company has outlined a series of innovations that mean its latest chip can train a neural network with up to 120 trillion parameters. For reference, OpenAI’s revolutionary GPT-3 language model contains 175 billion parameters. The largest neural network to date, which was trained by Google, had 1.6 trillion.