AstraZeneca Plc shares rose after trial data showed Tagrisso slowed disease progression in patients with advanced lung cancer in another win for the pharmaceutical giant’s blockbuster drug.
AstraZeneca Plc shares rose after trial data showed Tagrisso slowed disease progression in patients with advanced lung cancer in another win for the pharmaceutical giant’s blockbuster drug.

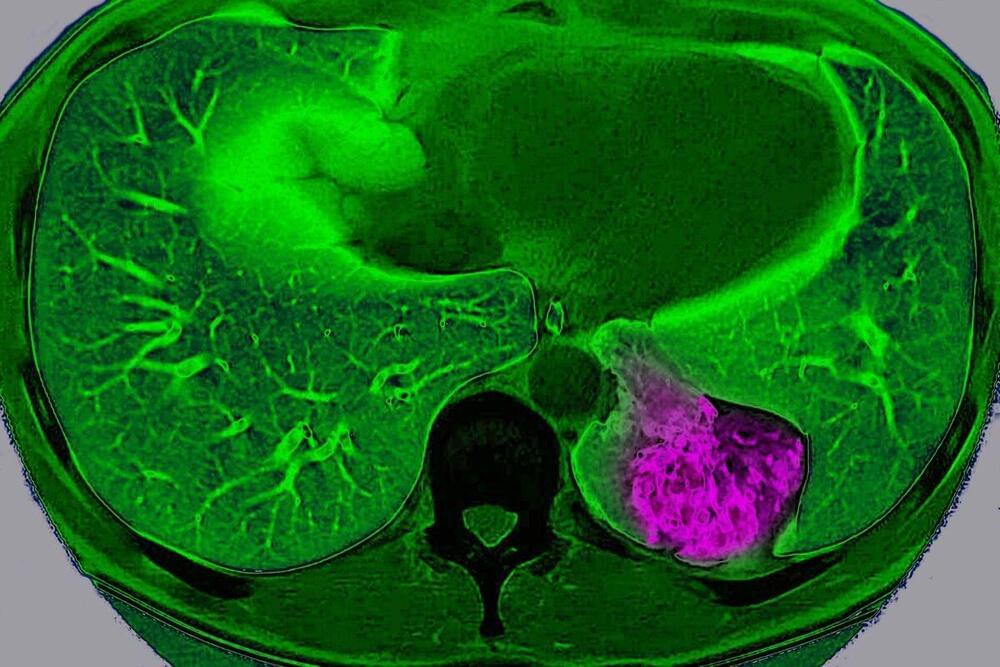
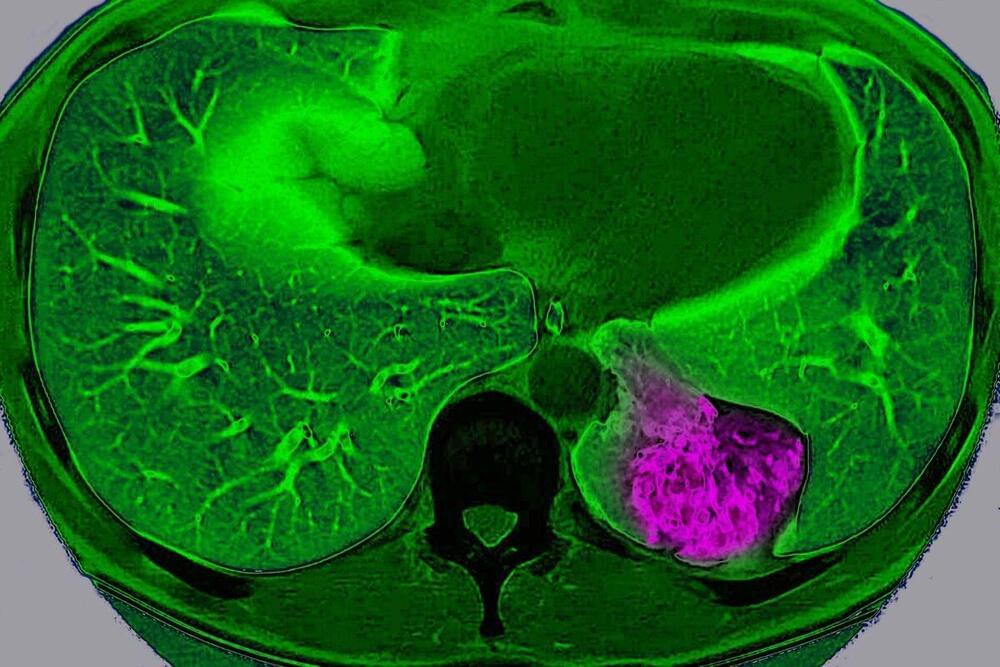
Excess amounts of vitamin B3 — which is found in meat, fish, nuts, and fortified cereals and breads — may trigger inflammation and damage blood vessels.
Non-personalized content and ads are influenced by things like the content you’re currently viewing and your location (ad serving is based on general location). Personalized content and ads can also include things like video recommendations, a customized YouTube homepage, and tailored ads based on past activity, like the videos you watch and the things you search for on YouTube. We also use cookies and data to tailor the experience to be age-appropriate, if relevant.
Select “More options” to see additional information, including details about managing your privacy settings. You can also visit g.co/privacytools at any time.
Genetic Engineering and DNA alteration is an emerging technology with huge ramifications in the future, including potentially altering the DNA of adult humans, not just embryos or plants \& animals.
Try Dashlane here: https://www.dashlane.com/isaacarthur.
Get 10% off now with my promo code: isaacarthur.
Visit our Website: http://www.isaacarthur.net.
Join Nebula: https://nebula.tv/videos/isaacarthur–…
Support us on Patreon: / isaacarthur.
Support us on Subscribestar: https://www.subscribestar.com/isaac-a…
Facebook Group: / 1583992725237264
Reddit: / isaacarthur.
Twitter: / isaac_a_arthur on Twitter and RT our future content.
SFIA Discord Server: / discord.
Listen or Download the audio of this episode from Soundcloud: Episode’s Audio-only version:
/ dna-manipulation-in-living-subjects.
Episode’s Narration-only version: / dna-manipulation-in-living-subjects-narrat…
Credits:
DNA Manipulation in Living Subjects (original title)
Genetically Altering Living Organisms.
Episode 227; Feb 27, 2020
Writers:
Isaac Arthur.
Editors:
METROPOLIS a film by Fritz Lang — Version “Cobra — 2022” — 4K Remastered — 60fps — Also available on UHD 4K download!
Re-edited \& Reframed — New Time Mapping (some technical considerations below):
New Intertitles \& English Adaptation — Screenplay by Maximianno Cobra.
Music — Original Score and Soundtrack (2022)
“Metropolis — Ordo ab Chao” Symphony.
by Maximianno Cobra.
Recorded by TEMPUS Collection — Europa Philharmonia Orchestra.
www.tempuscollection.com.
IMAGINARY STREAMS
Post-production \& Mastering.
www.imaginarystreams.com.

For decades, robots.txt governed the behavior of web crawlers.
As unscrupulous AI companies crawl for more and more data, the basic social contract of the web is falling apart.

The Cocoa Press isn’t an easy 3D printer — but how many let you eat the results?
I hate to be the bearer of bad-for-the-waistline news, but yes — you can now buy a 3D printer that prints chocolate.
The Cocoa Press is a 3D printer that prints chocolate. It costs $1,499 as a DIY kit, and $3,995 prebuilt. It’s shipping now.

Stephanie Song, formerly on the corporate development and ventures team at Coinbase, was often frustrated by the volume of due diligence tasks she and her team had to complete on a daily basis.
Dili is a new, Y Combinator-backed startup that aims to automate different aspects of the due diligence process using AI.

Although I like to write about future predictions for the world of technology and business, I’m usually focused on what’s coming up in the next five years.
But it’s also worth taking a longer view. I believe that in 10 years’ time, the AI that’s a part of everyday life will be as far evolved from today’s AI as today’s internet is from the internet of the early days.
In his excellent book The Coming Wave, Mustafa Suleyman notes that every wave of technology-driven change – from the combustion engine to the internet – has revolutionized society in a shorter time span than the previous wave. So, I don’t think we’ll have to wait 30 or even 20 years until AI is utterly engrained in all aspects of life.
Instead, let’s look ahead just 10 years to 2034. Halfway through the next decade, a lot will have changed, but what will AI look like? Here’s what I think!

New plasma stealth device targets specific areas, not entire aircraft.
Chinese scientists develop plasma stealth device, hiding military aircraft from radar, focusing on shielding specific areas, potentially changing stealth technology.