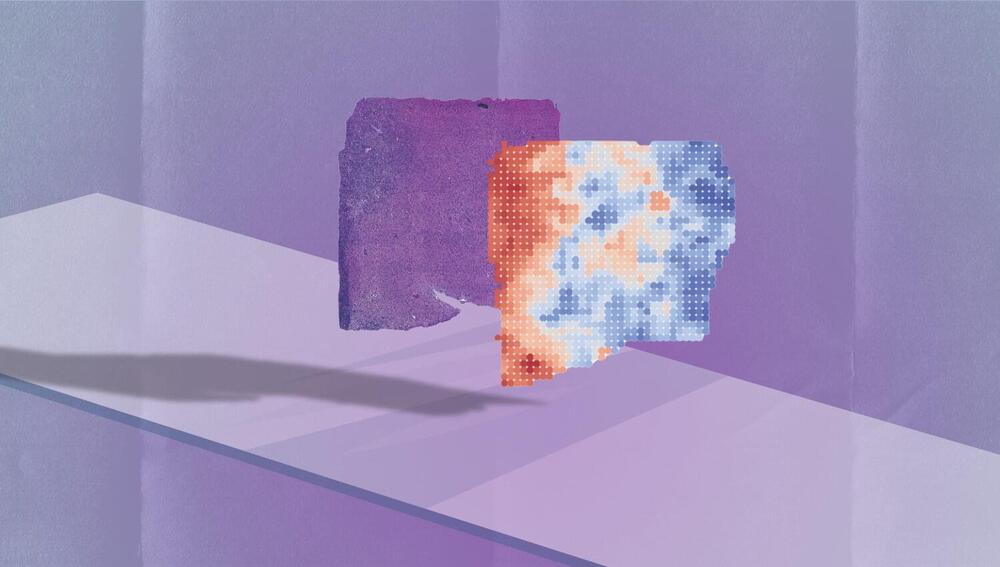
Water, a molecule essential for life, exhibits unusual properties—referred to as anomalies—that define its behavior. Despite extensive study, many mysteries remain about the molecular mechanisms underlying these anomalies that make water unique. Deciphering and replicating this distinctive behavior across various temperature ranges remains a significant challenge for the scientific community.
Now, a study presents a new theoretical model capable of overcoming the limitations of previous methodologies to understand how water behaves in extreme conditions. The paper, featured on the cover of The Journal of Chemical Physics, is led by Giancarlo Franzese and Luis Enrique Coronas, from the Faculty of Physics and the Institute of Nanoscience and Nanotechnology of the University of Barcelona (IN2UB).
The study not only broadens our understanding of the physics of water, but also has implications for technology, biology and biomedicine, in particular for addressing the treatment of neurodegenerative diseases and the development of advanced biotechnologies.