The ancient genes prompted the mice to develop larger heads and several other traits.



Breast cancer (BC) is the most common cancer in the world as well as the most common malignancy in Korean women, and the incidence continues to increase [1, 2]. Due to increased early detection with cancer screening programs and advances in systemic treatment such as chemotherapy, anti-hormone therapy, and human epidermal growth factor 2 (HER2)-targeted therapy, more patients are surviving after treatment for BC [3].
Current surveillance guidelines for follow-up after a diagnosis of BC recommend regular mammography (MMG) and physical examinations as well as further symptom-related laboratory tests and imaging tests, such as computed tomography (CT) or positron emission tomography-CT scans [4, 5]. These guidelines are based on data from clinical trials performed in the early 1990’s, which did not show any survival benefit with the early detection of distant metastasis [6, 7]. However, those clinical trials were mainly conducted using imaging modalities with poor sensitivity (e.g., chest X-ray), physical examinations with examiner-dependent variation of sensitivity (e.g., abdominal sonography), or procedures with limited specificity (e.g., bone scan), and did not include tumor markers (e.g., cancer antigen 15–3 [CA15-3]).
CA15-3 is a serum tumor marker for BC extensively used in clinical practice. CA15-3 is non-invasive, easily available, and a cost-effective tumor marker for immediate diagnosis, monitoring, and prediction of BC in early, advanced, and metastatic BC [8, 9, 10]. However, to the best of our knowledge, its clinical value within normal range has not been assessed. We hypothesized that an elevation of CA15-3 levels which were initially within normal ranges in patients with early BC could affect recurrence of BC; thus, the association between elevated CA15-3 levels and BC recurrence was analyzed in the present study.


The simulation of strongly interacting many-body systems is a key objective of quantum physics research, as it can help to test the predictions of physics theories and yield new valuable insight. Researchers at Quantinuum, a quantum computing company, recently simulated a simplified version of a well-known theoretical model, the so-called Sachdev-Ye-Kitaev (SYK) model, using a trapped-ion quantum computer and a previously introduced randomized quantum algorithm.
Their simulation, outlined in a paper published on the arXiv preprint server, improves the present understanding of chaotic quantum systems that cannot be simulated using classical computers. In the future, their work could contribute to the simulation of other complex quantum systems and theoretical models.
“We were interested in the SYK model for two reasons: on one hand it is a prototypical model of strongly interacting fermions in condensed matter physics, and on the other hand it is the simplest toy model for studying quantum gravity in the lab via the holographic duality,” said Enrico Rinaldi, Lead R&D Scientist at Quantinuum and senior author of the paper.

Because of the “all-or-none” character of nervous activity, neural events and the relations among them can be treated by means of propositional logic. It is found that the behavior of every net can be described in these terms, with the addition of more complicated logical means for nets containing circles; and that for any logical expression satisfying certain conditions, one can find a net behaving in the fashion it describes. It is shown that many particular choices among possible neurophysiological assumptions are equivalent, in the sense that for every net behaving under one assumption, there exists another net which behaves under the other and gives the same results, although perhaps not in the same time. Various applications of the calculus are discussed.
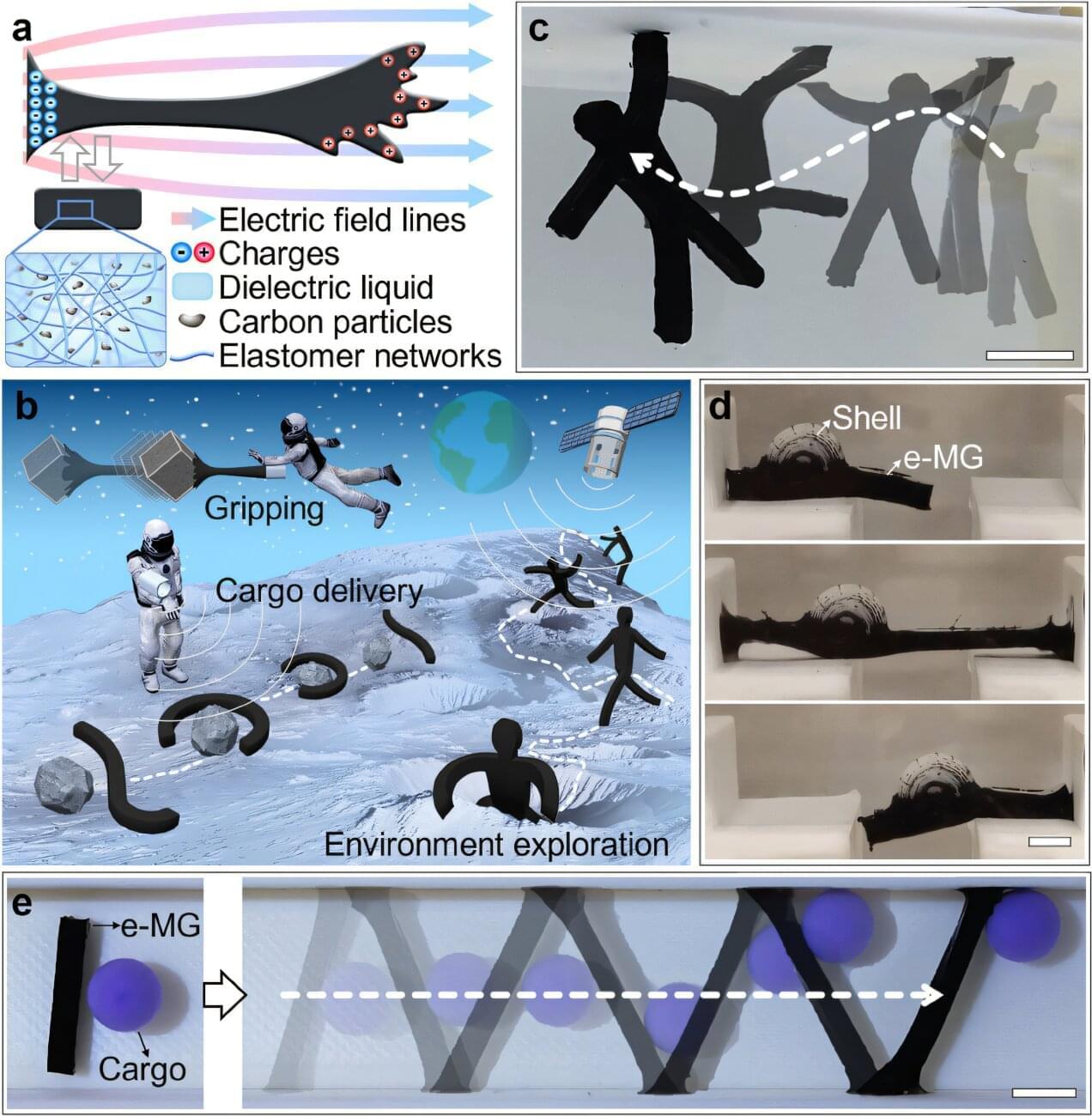
Researchers have invented a new super agile robot that can cleverly change shape thanks to amorphous characteristics akin to the popular Marvel anti-hero Venom.
The unique soft morphing creation, developed by the University of Bristol and Queen Mary University of London, is much more adaptable than current soft robots. The study, published in the journal Advanced Materials, showcases an electro-morphing gel jelly-like humanoid gymnast that can move from one place to another using its flexible body and limbs.
Researchers used a special material called electro-morphing gel (e-MG) which allows the robot to show shapeshifting functions, allowing them to bend, stretch, and move in ways that were previously difficult or impossible, through manipulation of electric fields from ultralightweight electrodes.
