With mechanical recycling, “if you mix the sandwich bag and the milk jug together and then try to remake an object from that, you can’t make a very good milk jug and you can’t make a very good sandwich bag,” he said. “We’re trying to bring the plastics back to the chemicals from which they’re made in the first place,” Hartwig said.
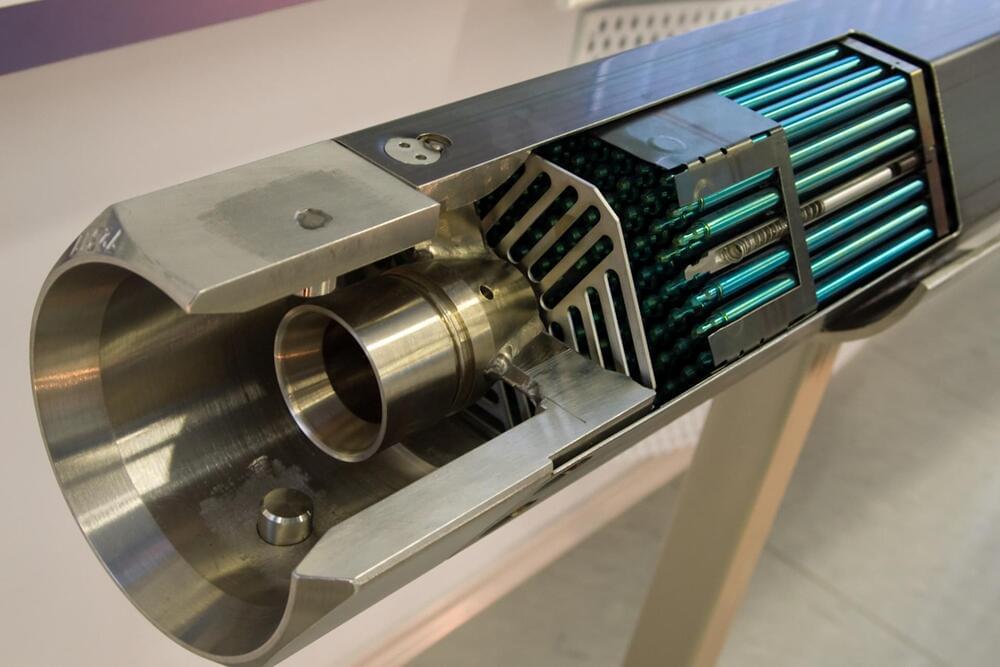
The researchers use a catalyst, a component of a chemical reaction that makes it go faster, to vaporize both polyethylene and polypropylene plastics — two of the largest volumes of plastics in existence — transforming the solid waste into gases.
The polymers are reduced to their chemical precursors, which can then be reconstructed. In a press release, the university said the process brings “a circular economy for plastics one step closer to reality.”