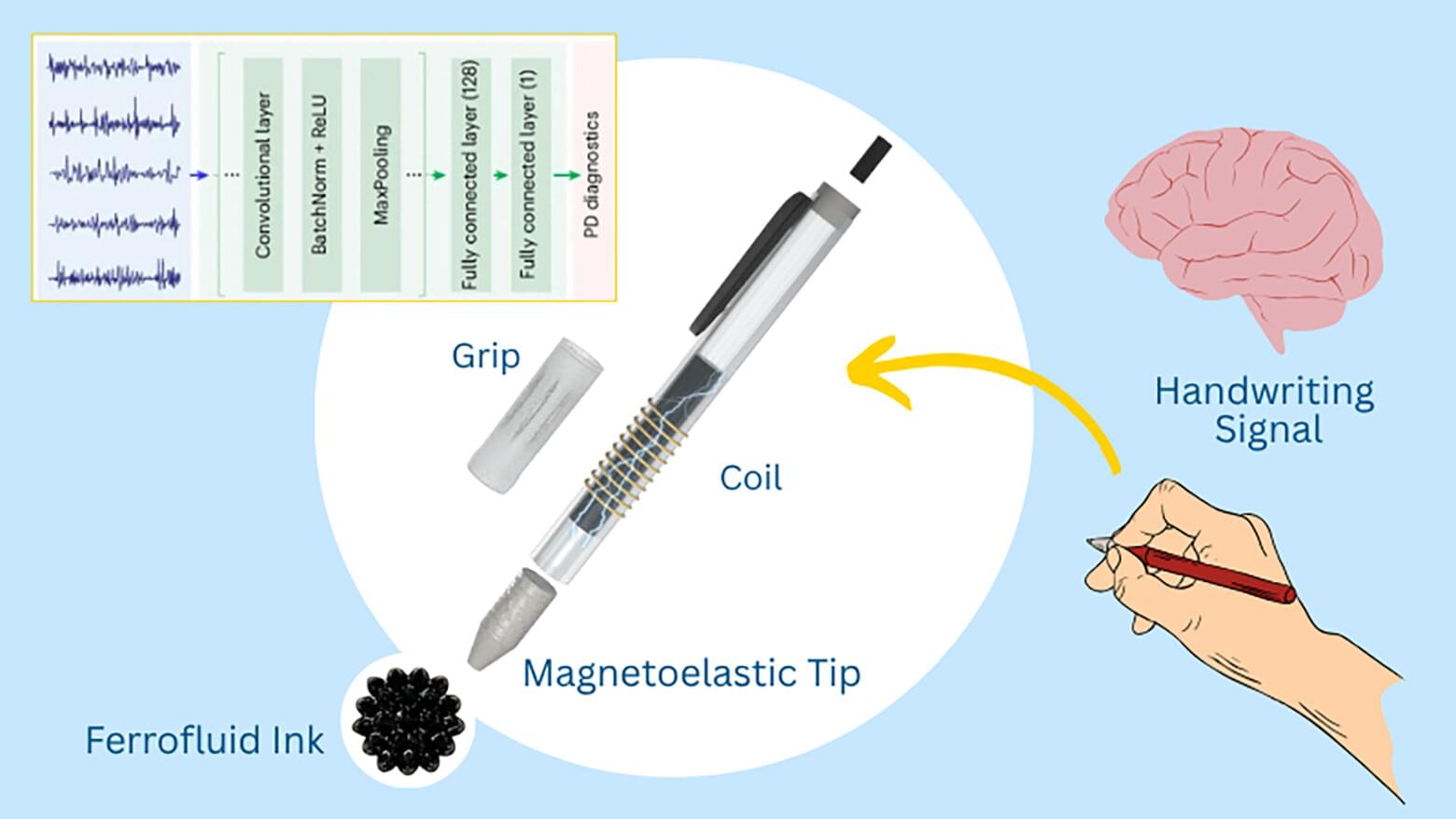
Every year, tens of thousands of people with signs of Parkinson’s disease go unnoticed until the incurable neurodegenerative condition has already progressed.
Motor symptoms, such as tremors or rigidity, often emerge only after significant neurological damage has occurred. By the time patients are diagnosed, more than half of their dopamine-producing neurons may already be lost. This kind of diagnostic delay can limit treatment options and slow progress on early-stage interventions.
While there are existing tests to detect biomarkers of Parkinson’s, including cell loss in the brain and inflammatory markers in blood, they typically require access to specialists and costly equipment at major medical centers, which may be out of reach for many.