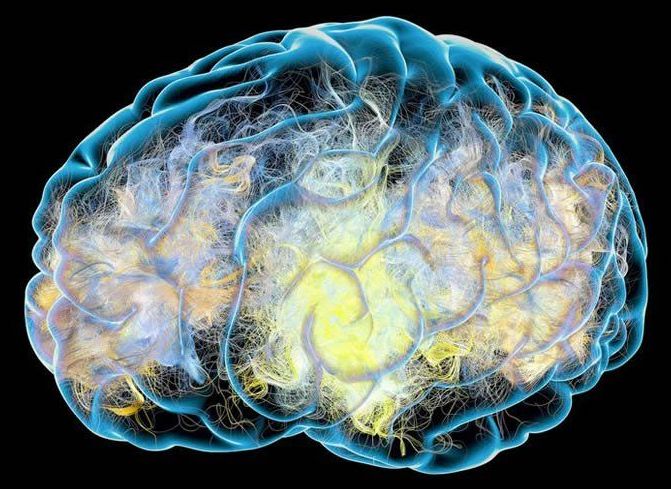
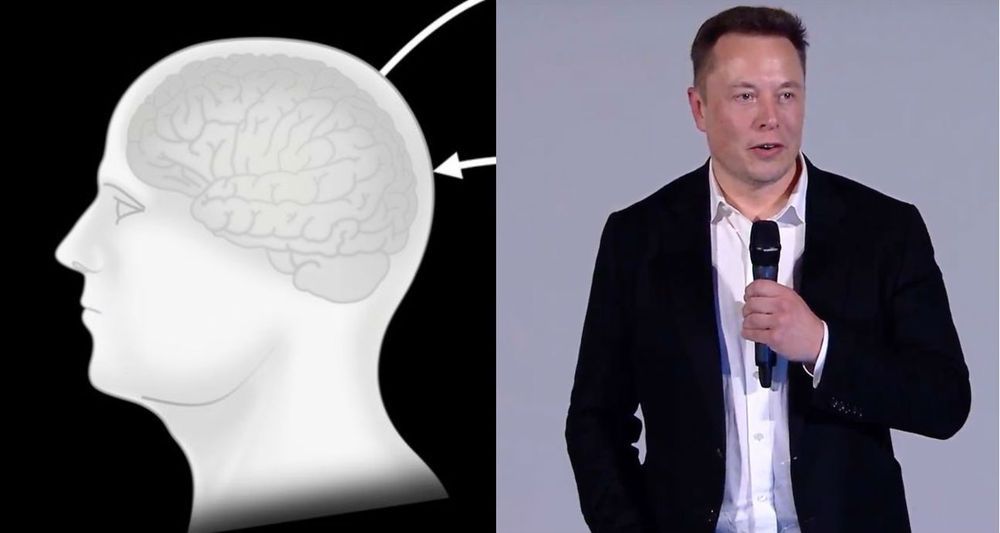
Elon Musk’s Neuralink will likely show off its design for a brain-computer interface Friday evening. The concept it unveiled last summer involves surgically implanting it into the brain to detect the activity of neurons. The US military also wants to develop a brain-computer interface, as we explain in this story from October. But here’s the kicker: no surgery required—and the device could be put on and taken off like a helmet or headband.
In August, three graduate students at Carnegie Mellon University were crammed together in a small, windowless basement lab, using a jury-rigged 3D printer frame to zap a slice of mouse brain with electricity.
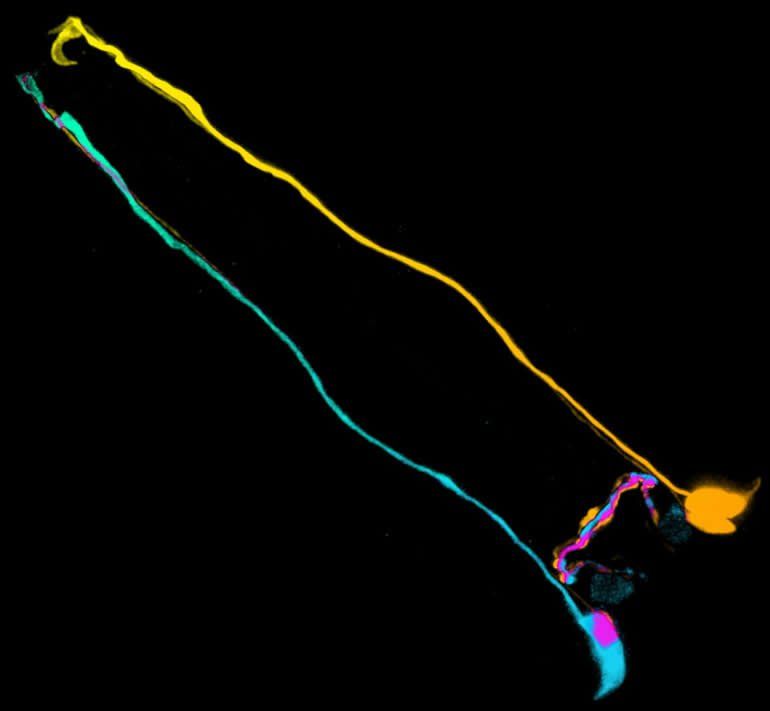
The brain fragment, cut from the hippocampus, looked like a piece of thinly sliced garlic. It rested on a platform near the center of the contraption. A narrow tube bathed the slice in a solution of salt, glucose, and amino acids. This kept it alive, after a fashion: neurons in the slice continued to fire, allowing the experimenters to gather data. An array of electrodes beneath the slice delivered the electric zaps, while a syringe-like metal probe measured how the neurons reacted. Bright LED lamps illuminated the dish. The setup, to use the lab members’ lingo, was kind of hacky.