Check out this short educational video in which I explain some super exciting research in the area of nanotechnology: gigadalton-scale DNA origami! I specifically discuss a journal article by Wagenbauer et al. titled “Gigadalton-scale shape-programmable DNA assemblies”.
Here, I explain an exciting nanotechnology paper “Gigadalton-scale shape-programmable DNA assemblies” (https://doi.org/10.1038/nature24651).
Though I am not involved in this research myself, I have worked in adjacent areas such as synthetic biology, nanotechnology-based tools for neuroscience, and gene therapy. I am endlessly fascinated by DNA origami and would love to use it in my own research at some point in the future.
I am a PhD candidate at Washington University in St. Louis and the CTO of the startup company Conduit Computing. I am also a published science fiction writer and a futurist. To learn more about me, check out my website: https://logancollinsblog.com/.

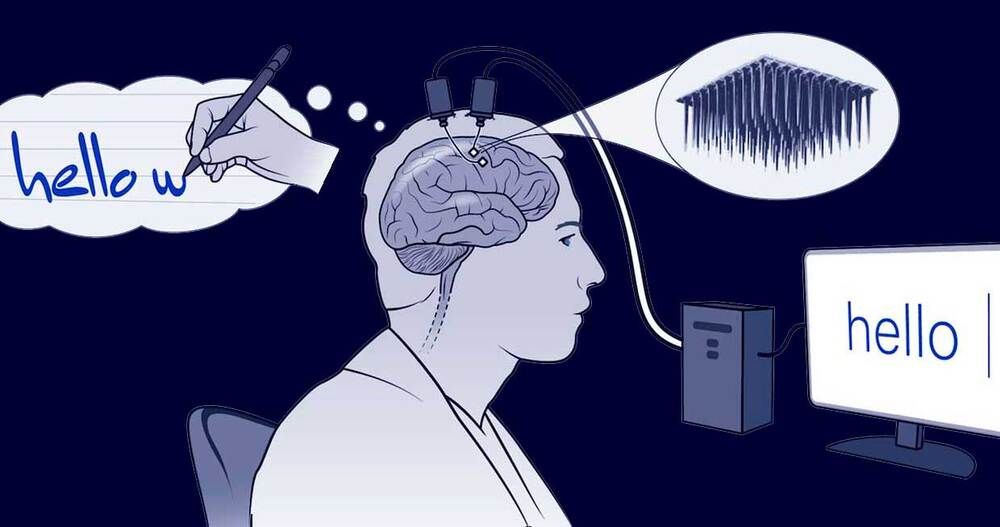 Erika Woodrum/HHMI/NatureTwo tiny arrays of implanted electrodes relayed information from the brain area that controls the hands and arms to an algorithm, which translated it into letters that appeared on a screen.
Erika Woodrum/HHMI/NatureTwo tiny arrays of implanted electrodes relayed information from the brain area that controls the hands and arms to an algorithm, which translated it into letters that appeared on a screen.