A new study in mouse models of Alzheimer’s suggests that replacing blood containing amyloid-beta with fresh, healthy blood, may have therapeutic potential.



From its very inception quantum mechanics troubled physicists. It seemed to challenge our conception of reality and lead to apparent contradictions. One of the founders of quantum mechanics, Ernst Heisenberg, questioned whether the theory offered a description of reality at all. Others, like Niels Bohr, claimed that somehow human consciousness played a role in the theory. In this interview, Carlo Rovelli explains Heisenberg’s anti-realist motivations, clarifies the role of the “observer” in quantum mechanics, and articulates his relational interpretation of the theory, according to which reality is a network of interactions.
Carlo Rovelli will debate Sabine Hossenfelder and Eric Weinsten in the FREE IAI Live event, ‘Quantum Physics and the End of Reality’ on July 25th. Learn more here.
The founders of quantum mechanics were very uncomfortable with its results – famously Einstein thought it an incomplete theory and quipped “God doesn’t play dice”, and Schrödinger abandoned physics altogether for biology. What was so radically different about quantum mechanics than classical physics that caused such discomfort to its own creators?

Summary: Researchers discovered a specific neurotransmitter that helps assign either positive or negative emotions to memories.
Source: Salk Institute.
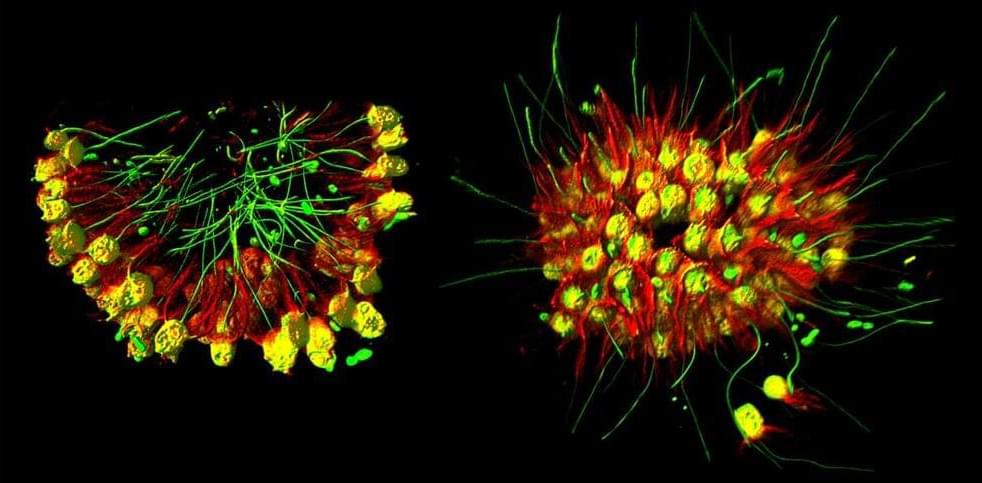
Researchers at the Salk Institute and colleagues have discovered the molecule in the brain responsible for associating good or bad feelings with a memory.

It’s all about a mutation of genome. Researchers from the University of California San Diego School of Medicine have discovered a set of human gene mutations that prevent cognitive decline and dementia in older adults, according to a new study published on July 9, 2022, in the journal Molecular Biology and Evolution. The scientists focused on one of the mutated genes and traced its evolution through its appearance in the human genome.
Interesting Engineering is a cutting edge, leading community designed for all lovers of engineering, technology and science.

😳!!!!!
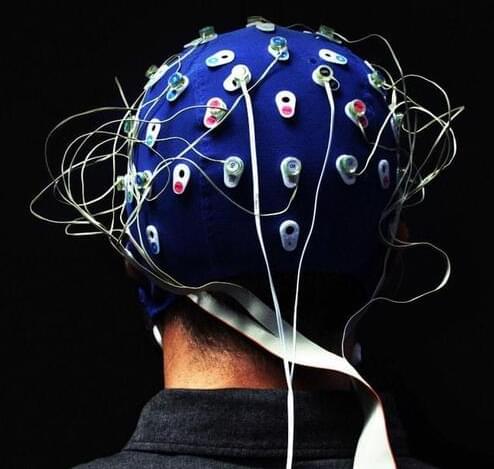
In a milestone that could turn sci-fi into fact, the first U.S. clinical trial of a brain implant that returns the power of communication to severely paralyzed people has begun. | In a milestone that could turn sci-fi into fact, the first U.S. clinical trial of a brain implant that returns the power…
Brain-computer interfaces have become a practical (if limited) reality in the US. Synchron says it has become the first in the country to implant a BCI in a human patient. Doctors in New York’s Mount Sinai West implanted the company’s Stentrode in the motor cortex of a participant in Synchron’s COMMAND trial, which aims to gauge the usefulness and safety of BCIs for providing hands-free device control to people with severe paralysis. Ideally, technology like Stentrode will offer independence to people who want to email, text and otherwise handle digital tasks that others take for granted.
Surgeons installed the implant using an endovascular procedure that avoids the intrusiveness of open-brain surgery by going through the jugular vein. The operation went “extremely well” and let the patient return home 48 hours later, according to Synchron. An ongoing Australian trial has also proven successful so far, with four patients still safe a year after receiving their implants.
It may take a long time before doctors can offer Synchron’s BCIs to patients. The company received FDA approval for human trials in July 2021, and it’s still expanding the COMMAND trial as of this writing. Still, the US procedure represents a significant step toward greater autonomy for people with paralysis. It also represents a competitive victory — Elon Musk’s Neuralink has yet to receive FDA permission for its own implant.