Contrary to the commonly-held view, the brain does not have the ability to rewire itself to compensate for the loss of sight, an amputation or stroke, for example, say scientists from the University of Cambridge and Johns Hopkins University.
Meta, the parent company of Facebook, has made a groundbreaking development in brain-computer interface technology. They have unveiled an AI system that can decode visual representations and even “hear” what someone is hearing by studying their brainwaves. These advancements in brain-machine interface technology have the potential to transform our relationship with artificial intelligence and its potential applications in healthcare, communication, and virtual reality.
The University of Texas at Austin has developed a new technology that can translate brain activity into written text without surgical implants. This breakthrough uses functional Magnetic Resonance Imaging (fMRI) scan data to reconstruct speech. An AI-based decoder then creates text based on the patterns of neuronal activity that correspond to the intended meaning. This new technology could help people who have lost the ability to speak due to conditions such as stroke or motor neuron disease.
Despite the fMRI having a time lag, which makes tracking brain activity in real-time challenging, the decoder was still able to achieve impressive accuracy. The University of Texas researchers faced challenges in dealing with the inherent “noisiness” of brain signals picked up by sensors, but by employing advanced technology and machine learning, they successfully aligned representations of speech and brain activity. The decoder works at the level of ideas and semantics, providing the gist of thoughts rather than an exact word-for-word translation. This study marks a significant advance in non-invasive brain decoding, showcasing the potential for future applications in neuroscience and communication.
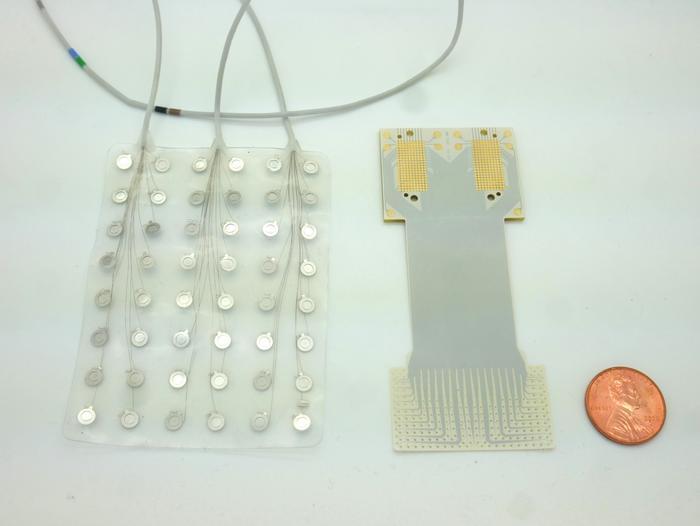
A speech prosthetic developed by a collaborative team of Duke neuroscientists, neurosurgeons, and engineers can translate a person’s brain signals into what they’re trying to say.
Year 2015 face_with_colon_three
A brain-computer interface lets a quadriplegic woman pilot an F-35 flight simulator with the power of her mind alone.

Protein indicators of subclinical peripheral heath in plasma were linked with markers of Alzheimer’s disease and neurodegeneration, cross-sectional proteomic analyses showed.
Greater protein-based risk for cardiovascular disease, heart failure mortality, and kidney disease was associated with plasma biomarkers of amyloid-beta, phosphorylated tau181 (p-tau181), neurofilament light (NfL, a measure of neuronal injury), and glial fibrillary acidic protein (GFAP, a measure of astrogliosis), even in people without cardiovascular or kidney disease, reported Keenan Walker, PhD, of the National Institute on Aging in Baltimore, and co-authors.
Proteomic indicators of body fat percentage, lean body mass, and visceral fat also were tied to p-tau181, NfL, and GFAP, Walker and colleagues wrote in the Annals of Neurology.

The sleep-wake cycle is among the most well-known circadian rhythms in the body and is severely affected in Alzheimer’s disease (AD). “Eighty percent of patients with AD suffer dysregulation or disruption of circadian rhythms, and the obvious clinical manifestations are the sleep-wake reversals,” Desplats said. “These patients are very sleepy during the day, agitated during the night, more confused, and sometimes aggressive.”
The feeding-fasting cycle is one of the strongest signals you can send the body to entrain the circadian clock.-Paula Desplats, University of California, San Diego
In a recent study published in Cell Metabolism, Desplats’s team used mice that are genetically engineered to develop AD to test whether intermittent fasting improves circadian rhythm abnormalities.3 Rather than restricting calories or making dietary changes, they simply limited food access to a defined six-hour daily window. They found that time-restricted eating improved sleep, metabolism, memory, and cognition, and reduced brain amyloid deposits and neuroinflammatory gene expression. “Many of the genes that are affected in AD are rhythmically expressed in the brain, meaning that they are in direct relation with the circadian clock and are involved in functions that are fundamental to AD pathology,” Desplats said. Intermittent fasting restored the rhythmic activity of these genes, but the real surprise was the extent to which it mitigated brain amyloid deposits and improved cognition and sleep-wake behaviors. “I didn’t expect that it will have such a dramatic impact on pathology,” Desplats said.
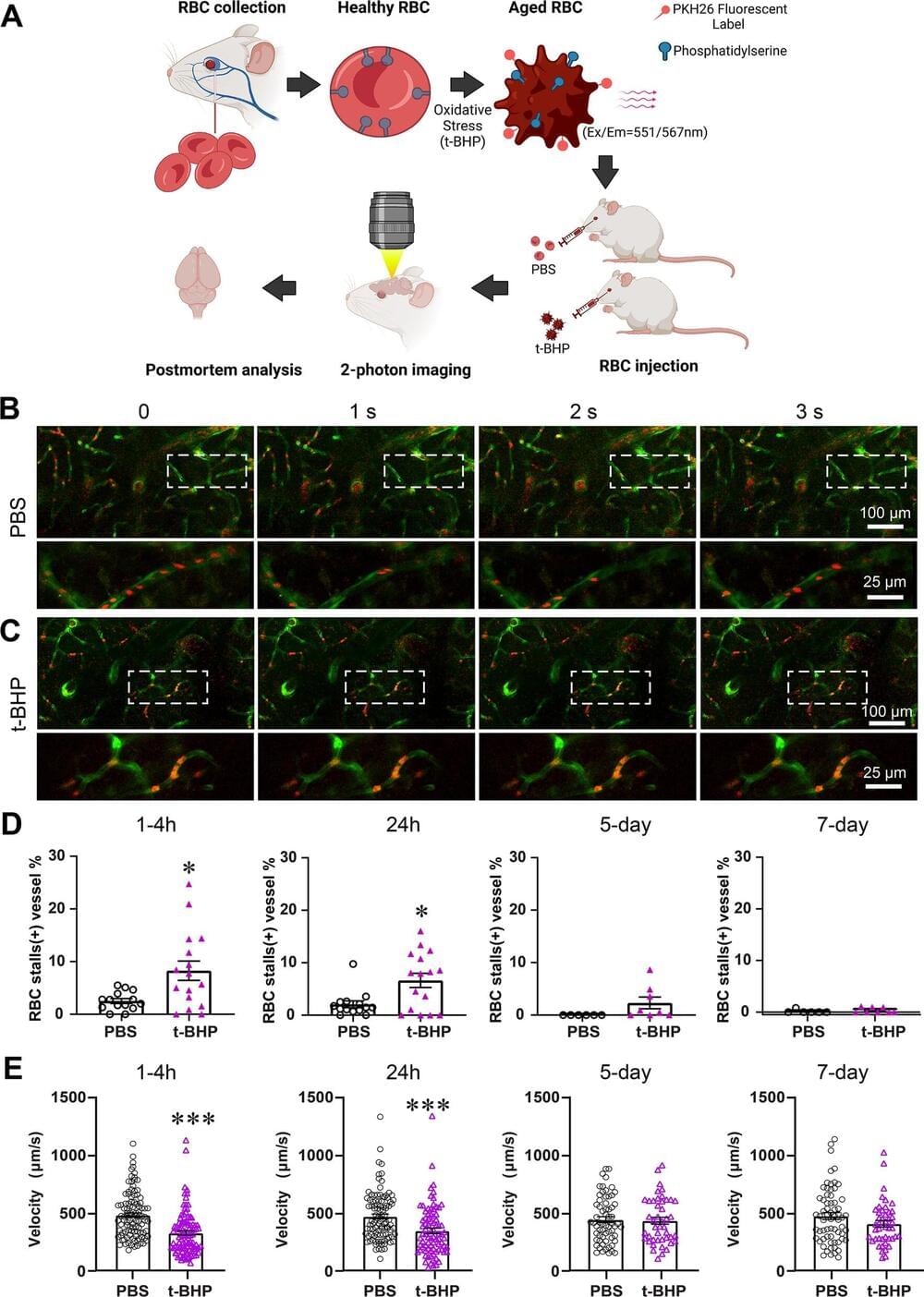
A first-of-its-kind study led by the University of California, Irvine has revealed a new culprit in the formation of brain hemorrhages that does not involve injury to the blood vessels, as previously believed. Researchers discovered that interactions between aged red blood cells and brain capillaries can lead to cerebral microbleeds, offering deeper insights into how they occur and identifying potential new therapeutic targets for treatment and prevention.
The findings, published online in the Journal of Neuroinflammation, describe how the team was able to watch the process by which red blood cells stall in the brain capillaries and then observe how the hemorrhage happens. Cerebral microbleeds are associated with a variety of conditions that occur at higher rates in older adults, including hypertension, Alzheimer’s disease and ischemic stroke.
“We have previously explored this issue in cell culture systems, but our current study is significant in expanding our understanding of the mechanism by which cerebral microbleeds develop,” said co-corresponding author Dr. Mark Fisher, professor of neurology in UCI’s School of Medicine. “Our findings may have profound clinical implications, as we identified a link between red blood cell damage and cerebral hemorrhages that occurs at the capillary level.”
Advancements in genetic engineering, gene therapies, and anti-aging research may eventually allow for age reversal and the restoration of youthful health and longevity.
What is the key idea of the video?
—The key idea is that advancements in genetic engineering and anti-aging research may eventually allow for age reversal and the restoration of youthful health and longevity.
How can aging be reversed?
—Aging can be reversed through rejuvenating the brain, restoring memories and learning abilities, and addressing the loss of inherited information through genetic engineering and epigenetic reprogramming.
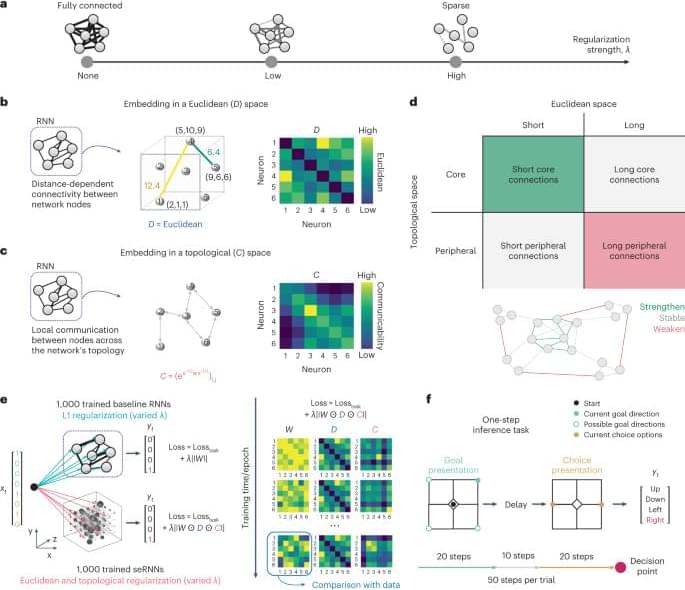
A fundamental question in neuroscience is what are the constraints that shape the structural and functional organization of the brain. By bringing biological cost constraints into the optimization process of artificial neural networks, Achterberg, Akarca and colleagues uncover the joint principle underlying a large set of neuroscientific findings.