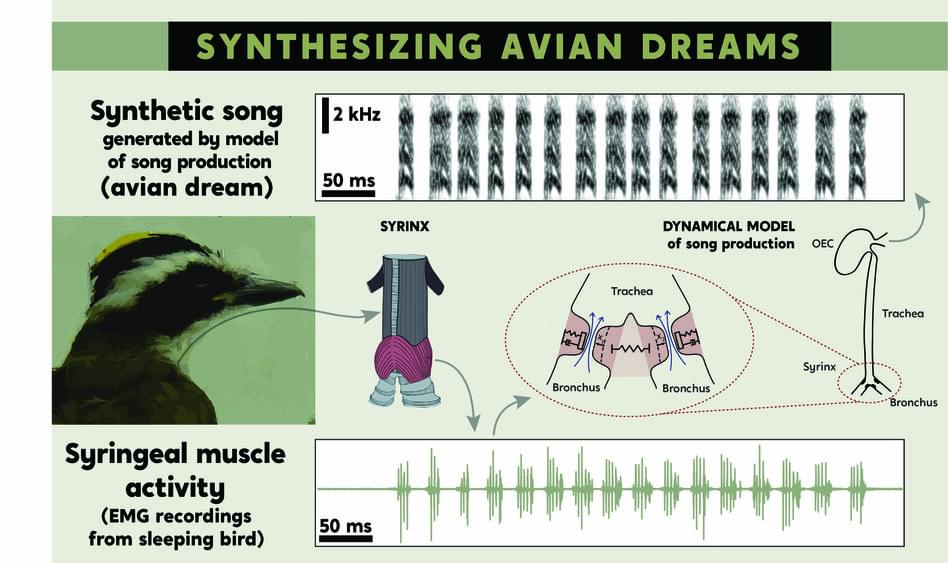
For more than 20 years, researchers have known that areas of birds’ brains dedicated to singing show neural patterns during sleep akin to the ones they use while awake and singing.
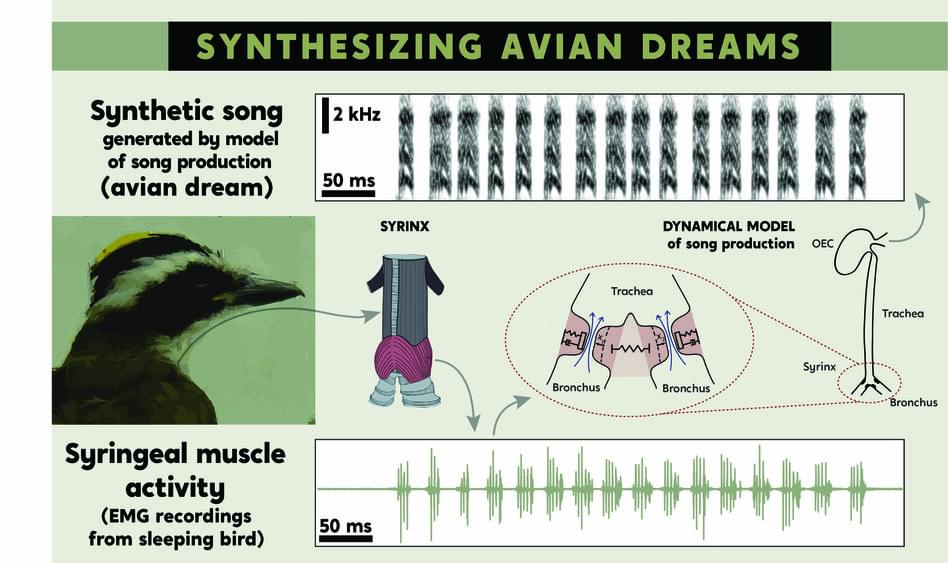
Physical touch from both humans and animals can reduce pain, feelings of depression, and anxiety in adults and children, according to a systematic review and meta-analysis published in Nature Human Behaviour. Read the paper:
This pre-registered systematic review and multilevel meta-analysis examined the effects of receiving touch for promoting mental and physical well-being, quantifying the efficacy of touch interventions for different ways of administration.
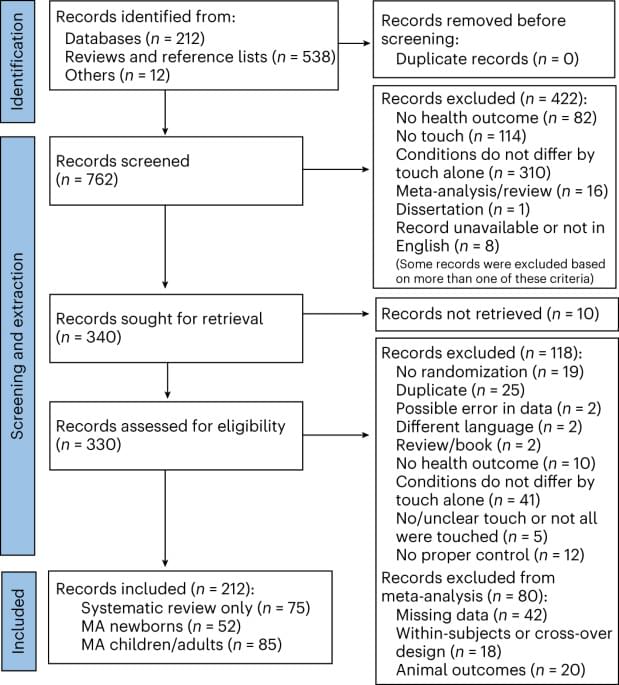
“This study is a first step in uncovering how we can mitigate risks of THC when used in medicine, and also is targeted at making cannabis safer for the general, non-therapeutic consumer,” said Dr. Tory Spindle.
Can cannabis be modified to decrease certain side effects, specifically anxiety, that is caused by tetrahydrocannabinol (THC)? This is what a recent study published in Drug and Alcohol Dependence hopes to address as a team of researchers led by the Johns Hopkins University School of Medicine investigated whether adding d-limonene, which is a known cannabis oil, to THC could help alleviate common feelings of anxiety or paranoia that cannabis users traditionally experience. This study holds the potential to help improve medicinal cannabis while decreasing risks to users of recreational cannabis, as well.
For the study, the researchers enlisted 20 healthy adult participants with an average age of 26 years old who completed 10 six-hour sessions involving them using vaporized THC alone (15 mg or 30 mg), vaporized d-limonene alone (1 mg or 5 mg), both together, and finally a placebo. The sessions were double-blinded, meaning both the researchers and participants were unaware who was vaporizing which sample.
While all 20 participated in nine sessions, 12 participants conducted the tenth session comprised of the higher dose of THC and an even higher dose of d-limonene at 15 mg. The goal of the sessions was to ascertain the overall drug effects, specifically vital signs, mood, and cognitive functions, along with blood and urine samples during and after each session to measure THC and d-limonene levels.
Parkinson’s disease is a neurodegenerative movement disorder that progresses relentlessly. It gradually impairs a person’s ability to function until they ultimately become immobile and often develop dementia. In the U.S. alone, over a million people are afflicted with Parkinson’s, and new cases and overall numbers are steadily increasing.
There is currently no treatment to slow or halt Parkinson’s disease. Available drugs don’t slow disease progression and can treat only certain symptoms. Medications that work early in the disease, however, such as Levodopa, generally become ineffective over the years, necessitating increased doses that can lead to disabling side effects.
Without understanding the fundamental molecular cause of Parkinson’s, it’s improbable that researchers will be able to develop a medication to stop the disease from steadily worsening in patients.
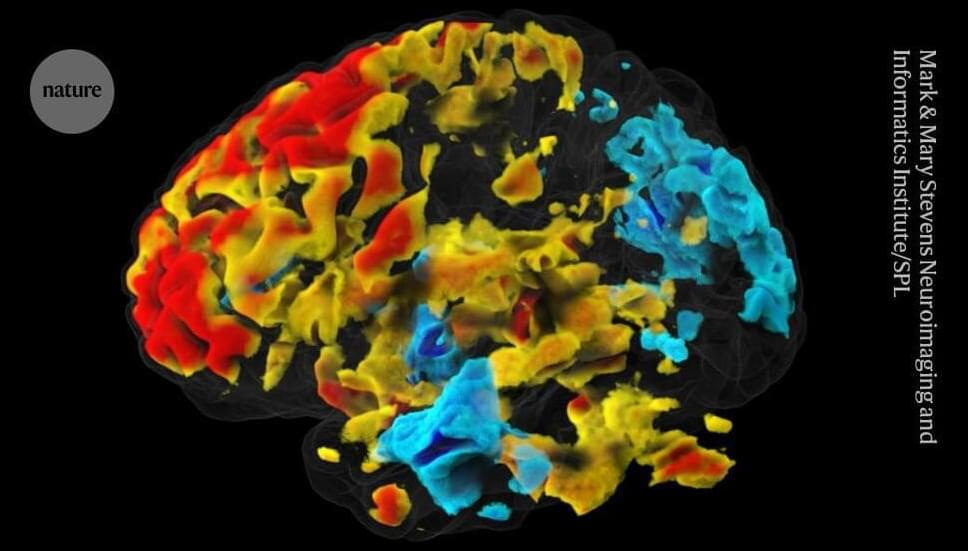
In conventional functional MRI (fMRI), researchers monitor changes in blood flow to different brain regions to estimate activity. But this response lags by at least one second behind the activity of neurons, which send messages in milliseconds.
Park and his co-authors said that DIANA could measure neuronal activity directly, which is an “extraordinary claim”, says Ben Inglis, a physicist at the University of California, Berkeley.
The DIANA technique works by applying minor electric shocks every 200 milliseconds to an anaesthetized animal. Between shocks, an MRI scanner collects data from one tiny piece of the brain every 5 milliseconds. After the next shock, another spot is scanned. The software stitches together data from all the spots, to visualize changes in an entire slice of brain over a 200-millisecond period. The process is similar to filming an action pixel by pixel, where the action would need to be repeated to record every pixel, and those recordings stitched together, to create a full video.
Is Chief Impact Officer for StartUp Health’s Alzheimer’s Moonshot (https://www.startuphealth.com/alzheimers), a new global initiative created to develop a collaborative innovation community alongside leading companies, research teams, and stakeholders, with a mission to accelerate progress in prevention, diagnosis, and management of Alzheimer’s disease and related dementias. With support from the Alzheimer’s Drug Discovery Foundation (ADDF) and Gates Ventures, StartUp Health is looking to break down silos and foster meaningful collaboration between mission-aligned founders, funders, and partners.
Dr. Ferrell also serves as Strategic Advisor, Davos Alzheimer’s Collaborative (https://www.davosalzheimerscollaborat…) which is building a global clinical trial network and technology platform that will link trial sites around the world.
Prior to these roles, Dr. Ferrell served almost three decades at multiple roles at Eli Lilly including as Global Head External Engagement, Alzheimer’s and Neurodegeneration, Chief Commercial Services Officer, and Vice President, Global Alzheimer’s Disease Platform Team Leader in Lilly BioMedicines, where her team were responsible for the late-stage development, global registration and launch of 4 late-stage assets including Solanezumab, Amyvid and AZD3293.
Dr. Ferrell received a DrPH, Public Health from Indiana University Richard M. Fairbanks School of Public Health, an MBA in General Management and a certificate in Public Management from the Stanford University Graduate School of Business, and a Bachelor of Arts degree in economics and management from DePauw University.
Dr. Ferrell was recognized with the Rising Star Award from the Healthcare Businesswomen’s Association and the Indianapolis Star Top 40 Under 40. She serves as a member of the World Dementia Council, a steering committee member of the Milken Institute Center for Aging Alliance for Dementia Care and National Minority Quality Forum (NMQF) Alzheimer’s Disease Index working groups, and a strategic reviewer for the Alzheimer’s Disease Drug Discovery Foundation Diagnostics Accelerator. She is also a member of the Indiana Chapter of the Healthcare Businesswomen’s Association; on the Boards of Directors for Alzheimer’s Research UK EDoN, Gates Ventures Alzheimer’s Disease Data Initiative, the Indiana Chapter of the Alzheimer’s Association, Stanford Associate Board of Governors, Indianapolis 500 Festival, and the Lebanon Area Boys \& Girls Club. She is a founding member of Women Against Alzheimer’s and Women of Impact Boone County; co-chair of the Women’s Leadership Council; the alumna sponsor of the Women in Economics and Business Program at DePauw University; a member of the Washington C. DePauw Society; a Tocqueville donor to United Way; an active supporter of Boone County Special Olympics and the Boone County Community Foundation.
2 Department of Neurobiology, Duke University, Durham, NC, United States.
3Center for Bioelectric Interfaces of the Institute for Cognitive Neuroscience, National Research University Higher School of Economics, Moscow, Russia.
4Department of Information and Internet Technologies of Digital Health Institute, I.M. Sechenov First Moscow State Medical University, Moscow, Russia.

In a global research effort, scientists have uncovered a relationship between metabolism problems in the brain and a range of neuropsychiatric and neurodegenerative disorders, from autism to Alzheimer’s disease and more.
Despite their diverse symptoms, these conditions – as well as depression, epilepsy, schizophrenia, intellectual disability, and bipolar disorder – all involve a degree of cognitive impairment and often share genetic or metabolic features, hinting at a common biological basis.
The extensive collaboration by the International Brain pH Project Consortium, involving 131 scientists from 105 labs in seven countries, identified changes in brain acidity and lactate levels in animals as key signs of this metabolic dysfunction.
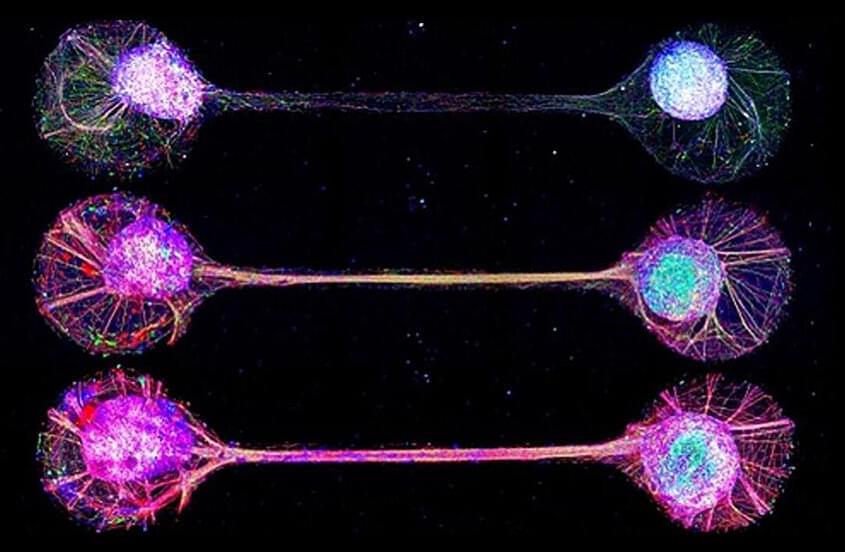
The idea of growing functioning human brain-like tissues in a dish has always sounded far-fetched, even to researchers in the field. Towards the future goal, a Japanese and French research team has developed a technique for connecting lab-grown brain-mimicking tissue in a way that resembles circuits in our brain.
The work appears in Nature Communications.
It is challenging to study exact mechanisms of the brain development and functions. Animal studies are limited by differences between species in brain structure and function, and brain cells grown in the lab tend to lack the characteristic connections of cells in the human brain. What’s more, researchers are increasingly realizing that these interregional connections, and the circuits that they create, are important for many of the brain functions that define us as humans.