Science has done many things that seem miraculous. Why not transfer your consciousness to a machine?


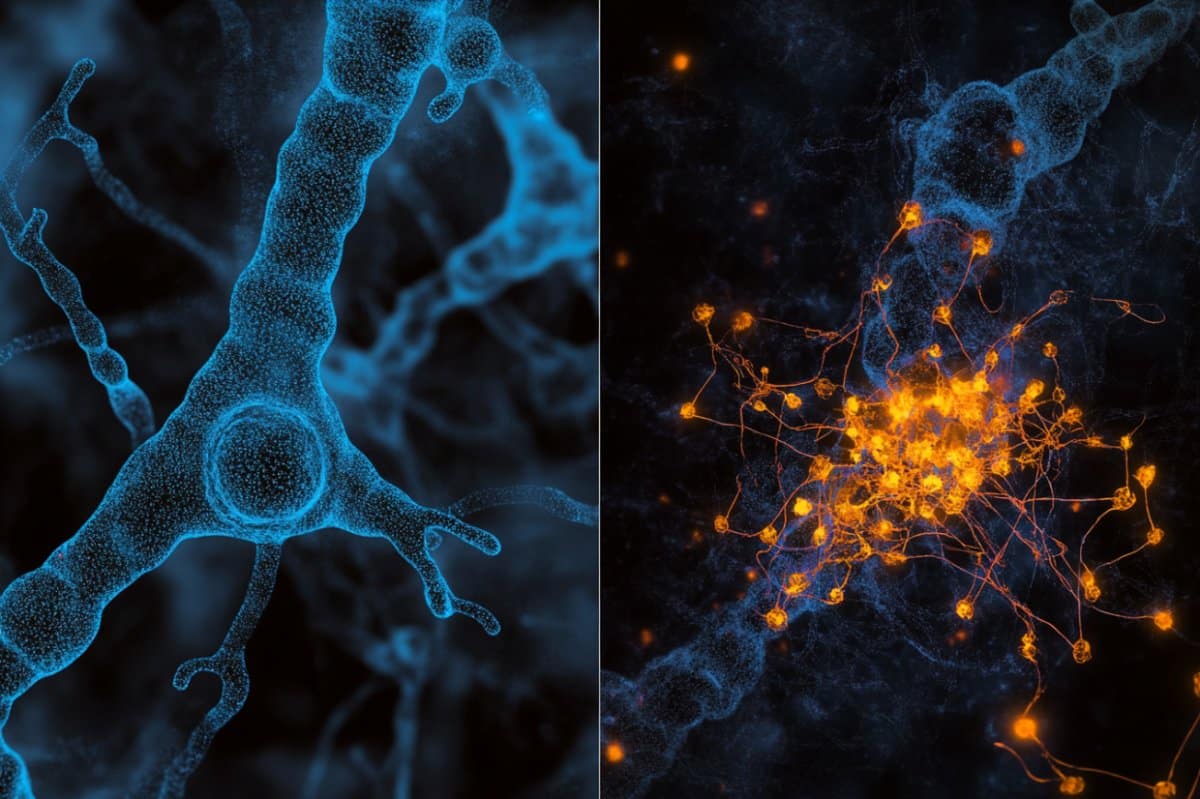
Most humans can recall specific events and past experiences for long periods of time. This capability, referred to as episodic memory, is known to be in great part supported by the activity of neurons in the hippocampus and medial temporal lobe.
Past neuroscience and psychology studies consistently found that episodic memory is associative. This essentially means that remembering one past event, for instance a graduation, can in many cases prompt people to also remember other related events, such as a party that celebrated the graduation.
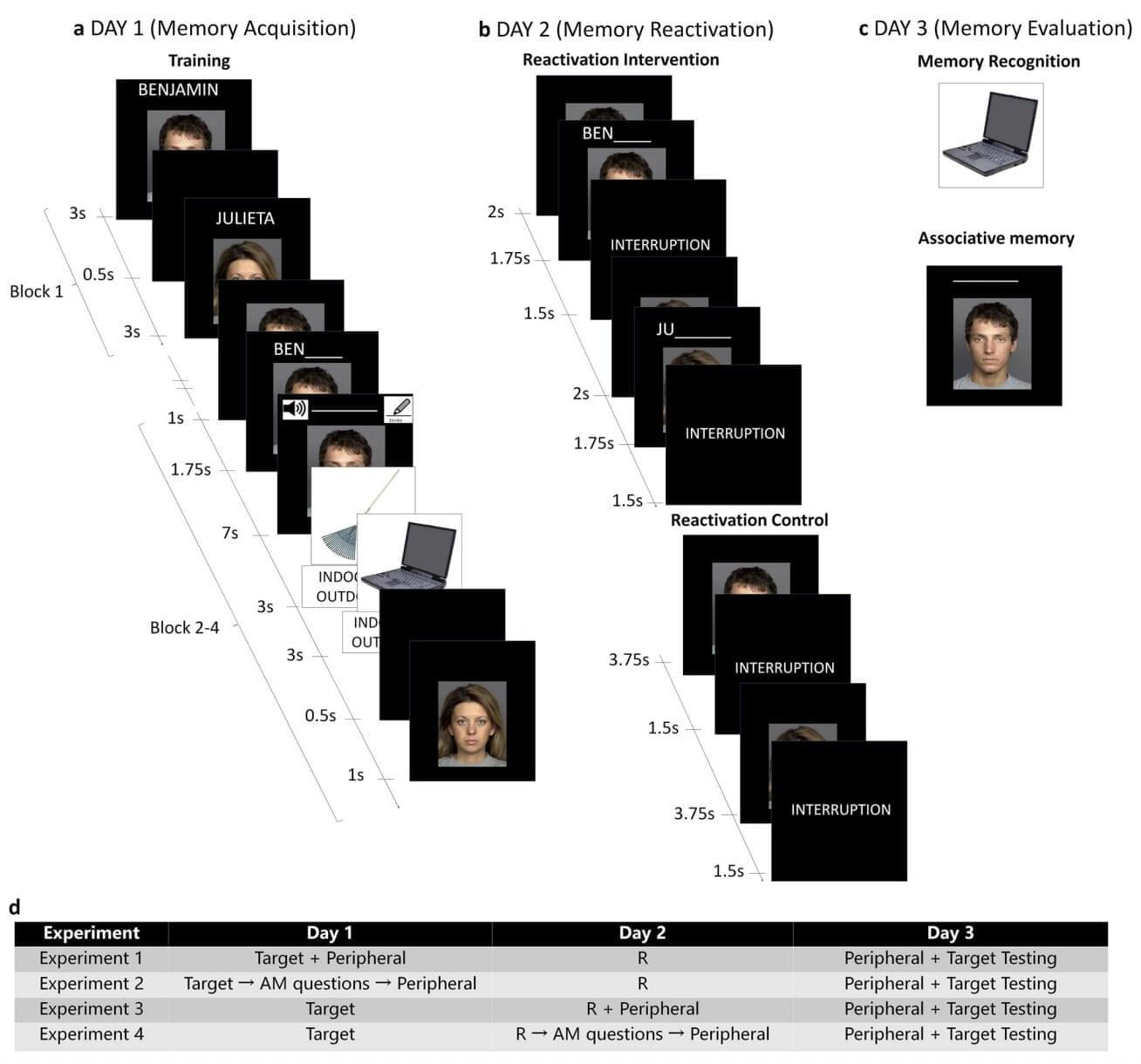
Researchers at Biología Molecular y Neurociencias (IFIByNE)-CONICET and the University of Buenos Aires recently carried out a new study exploring the possibility that the reactivation of specific episodic memories does not only help to strengthen those memories, but also the memories of other related events or experiences.
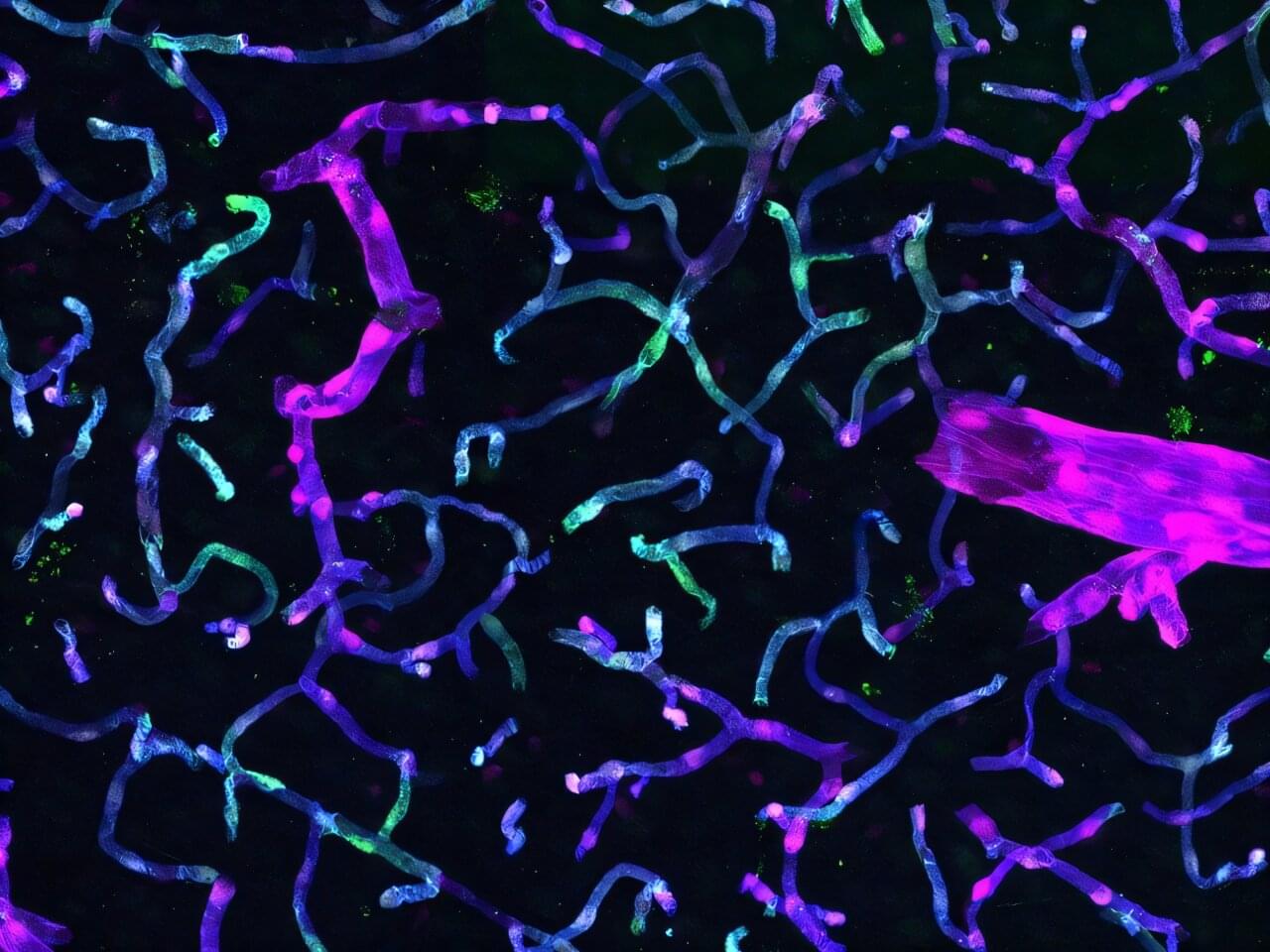
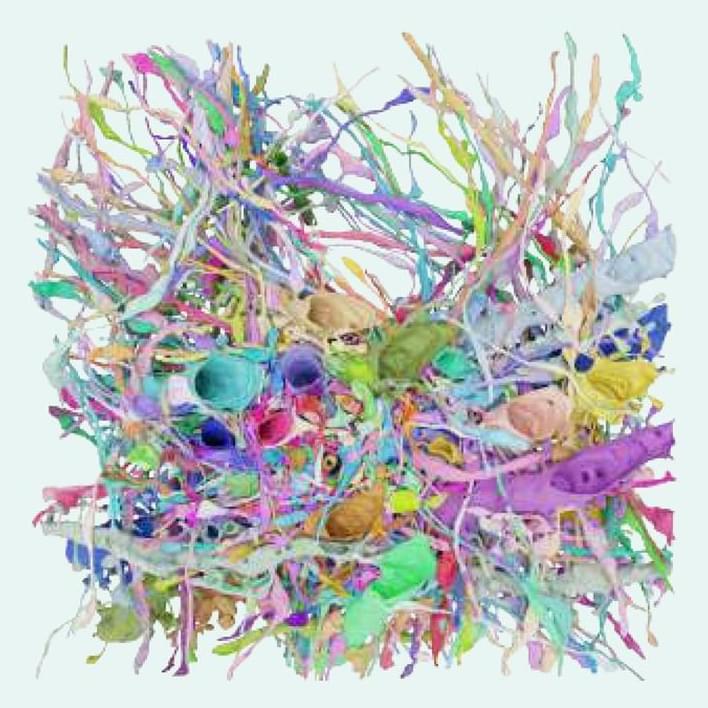
New studies stemming from the Armamentarium consortium outline findings that advance tools based on Adeno-associated virus (AAV) vectors. An announcement about the work explains how an AAV “acts like a shuttle capable of transporting specially designed DNA into the cell.”
Two of the studies on these AAV tools were conducted by collaborative teams organized by Xiangmin Xu, Ph.D., UC Irvine Chancellor’s Professor of anatomy and neurobiology and director of the campus’s Center for Neural Circuit Mapping.
“This Armamentarium’s collection of work enables new tools that help to deepen our understanding of the human central nervous system structure and function,” says Xu. “Our own brain-targeting technology could help treat Alzheimer’s disease and many other neurological disorders.”

Valve founder Gabe Newell’s neural chip company Starfish Neuroscience announced it’s developing a custom chip designed for next-generation, minimally invasive brain-computer interfaces—and it may be coming sooner than you think.
The company announced in a blog update that it’s creating a custom, ultra-low power neural chip in collaboration with R&D leader imec.
Starfish says the chip is intended for future wireless, battery-free brain implants capable of reading and stimulating neural activity in multiple areas simultaneously—a key requirement for treating complex neurological disorders involving circuit-level dysfunction. That’s the ‘read and write’ functions we’ve heard Newell speak about in previous talks on the subject.
Gabe Newell, co-founder of Valve, sat down with IGN for a chat about the company, the promise of VR, and Newell’s most bleeding edge project as of late, brain-computer interfaces (BCI).
Whenever I used to think about brain-computer interfaces (BCI), I typically imagined a world where the Internet was served up directly to my mind through cyborg-style neural implants—or basically how it’s portrayed in Ghost in the Shell. In that world, you can read, write, and speak to others without needing to lift a finger or open your mouth. It sounds fantastical, but the more I learn about BCI, the more I’ve come to realize that this wish list of functions is really only the tip of the iceberg. And when AR and VR converge with the consumer-ready BCI of the future, the world will be much stranger than fiction.
Be it Elon Musk’s latest company Neuralink —which is creating “minimally invasive” neural implants to suit a wide range of potential future applications, or Facebook directly funding research on decoding speech from the human brain—BCI seems to be taking an important step forward in its maturity. And while these well-funded companies can only push the technology forward for its use as a medical devices today thanks to regulatory hoops governing implants and their relative safety, eventually the technology will get to a point when it’s both safe and cheap enough to land into the brainpan’s of neurotypical consumers.
Although there’s really no telling when you or I will be able to pop into an office for an outpatient implant procedure (much like how corrective laser eye surgery is done today), we know at least that this particular future will undoubtedly come alongside significant advances in augmented and virtual reality. But before we consider where that future might lead us, let’s take a look at where things are today.