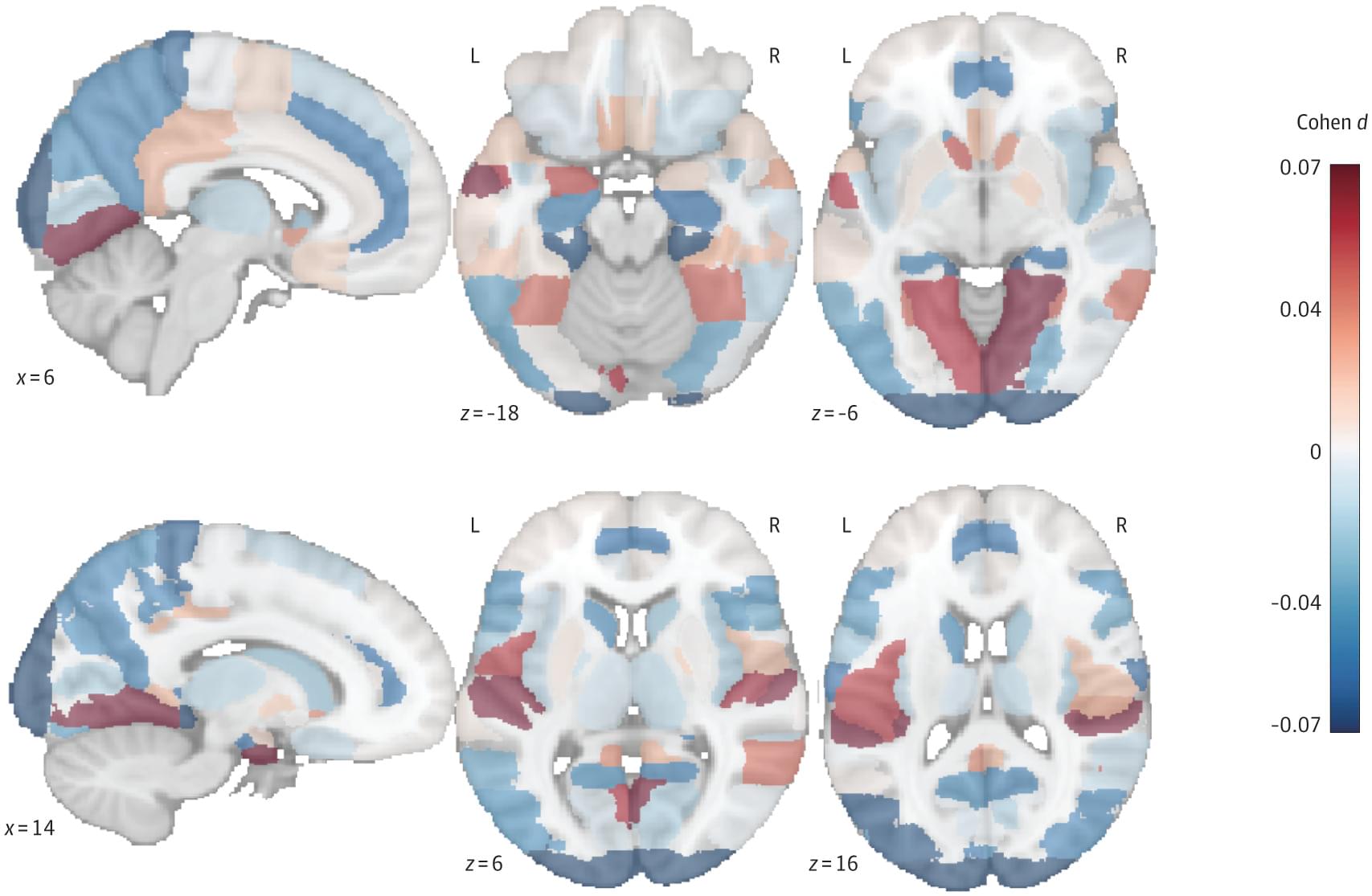
This cohort study investigates the association of active travel modes, such as walking and cycling, with dementia risk and brain structure.

A new study from The University of Texas at Arlington details a novel strategy for how the body clears out dead cells during stress, revealing unexpected roles for well-known stress-response genes—a discovery that could help scientists better understand diseases affecting the immune system, brain and metabolism.
“The body is constantly creating new cells and removing old cells once they die,” said Aladin Elkhalil, lead author of the study and a third-year doctoral student in the lab of Piya Ghose, assistant professor of biology at UT Arlington. “This removal of dead cells is just as important as creating new ones, because if the body is unable to rid itself of dead cells, it can lead to various health problems”
Published in PLOS Genetics, the study was conducted on the roundworm C. elegans by Dr. Ghose, Elkhalil and Alec Whited, another graduate student in the Ghose lab. This tiny, transparent organism is a widely used tool in genetic research because its see-through body allows scientists to observe live cell behavior, including how cells die. The research team took advantage of these unique features in several innovative ways.
How the brain largely maintains its function when neurons are lost—this is what researchers at the University Medical Center Mainz, the Frankfurt Institute for Advanced Studies (FIAS) and Hebrew University (Jerusalem) have deciphered. They show that neuronal networks in the cerebral cortex reorganize within a short period of time, with other nerve cells taking over the tasks of the lost neurons.
These findings could form the basis for future research into natural aging processes and neurodegenerative diseases such as Alzheimer’s or Parkinson’s. The study is published in the journal Nature Neuroscience.
Nerve cells (neurons) are the most important building blocks of the brain. They form the basis for all mental and physical functions such as thinking, feeling, movement, and perception. In the course of life, nerve cells in the brain can be lost for various reasons: They die off due to age-related processes, are damaged by toxins such as alcohol, or neurodegenerative diseases such as Alzheimer’s and Parkinson’s lead to a more rapid progressive loss of neurons.


Lithium-metal batteries have not hit the market yet, but if they do, they could be a solution to the everyday woes of the dwindling battery meter. They are cousins of the lithium-ion batteries found in legions of everyday electronic devices, but with the potential to hold twice as much power. Unfortunately, the lithium-metal battery’s limited number of recharges has been a major obstacle to their wide adoption.
A new study led by researchers at the California NanoSystems Institute at UCLA, or CNSI, however, might just help ratchet up the pace of progress. In the journal Science Advances, the team documented an imaging technique they invented that—for the first time ever—captures a lithium-metal battery as it charges, at a level of detail smaller than the wavelength of light.
The method, electrified cryogenic electron microscopy, or eCryoEM for short, yielded insights that may help guide the design of better lithium-metal batteries. Cultivating this progress with U.S.-based research could give the U.S. an edge in this successor technology to lithium-ion batteries, an industry currently dominated by Chinese enterprises. The study also holds promise for shedding light on mysteries in disciplines as far afield as neuroscience.
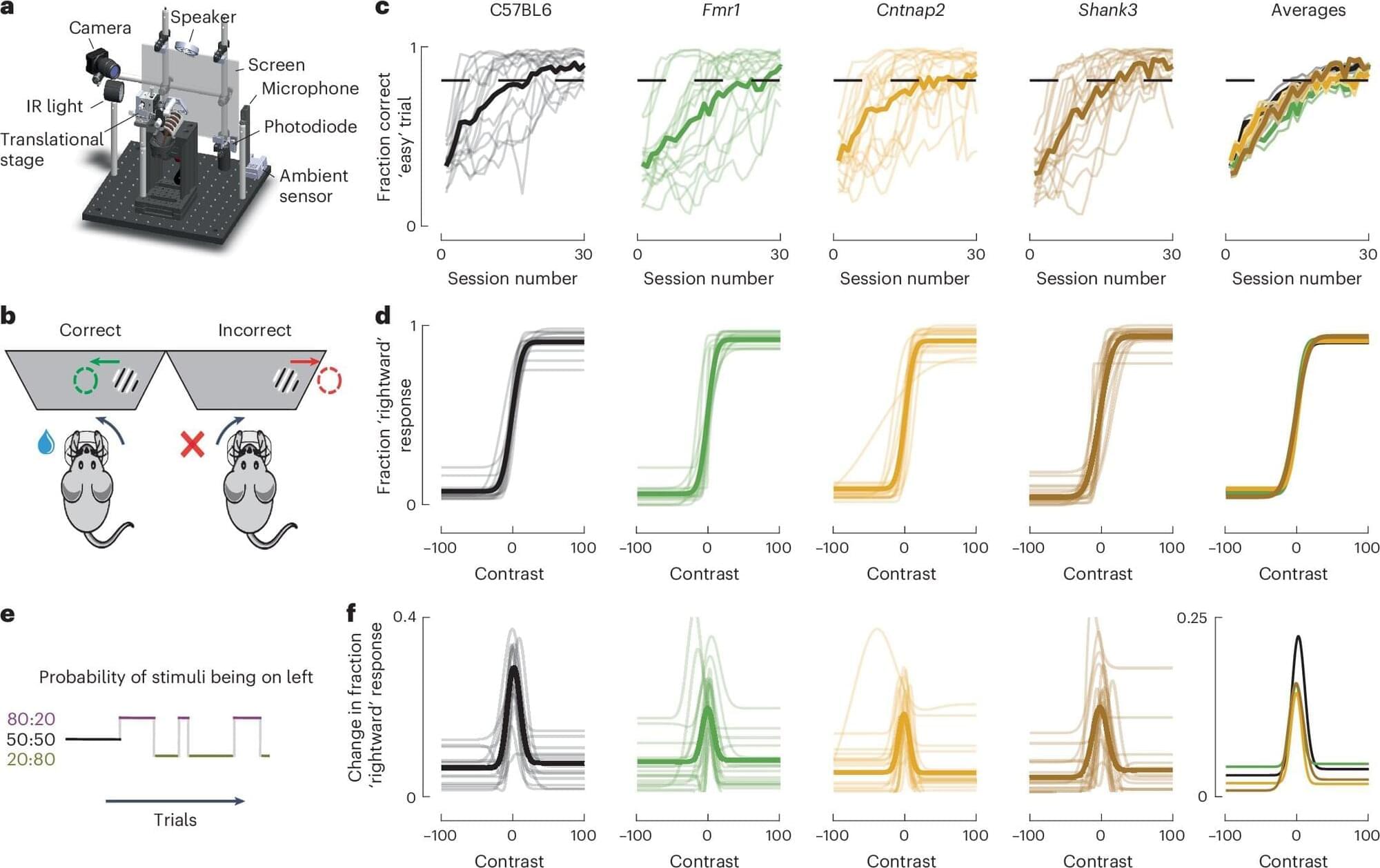
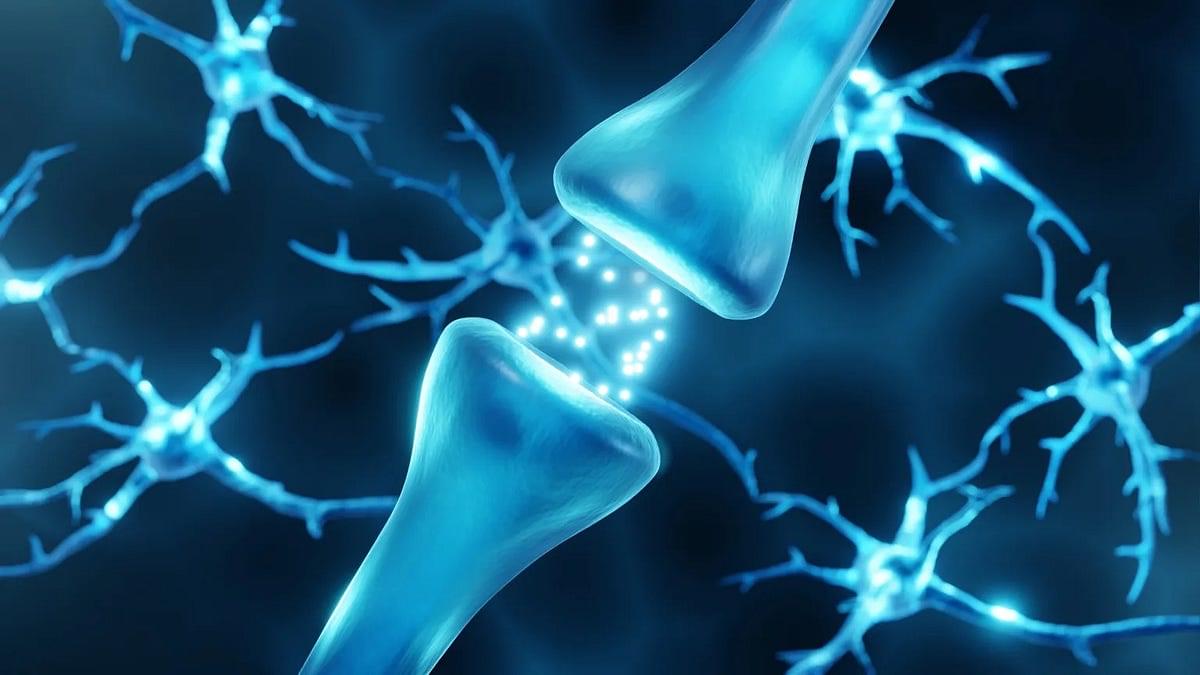
New research from the University of Minnesota Medical School suggests that different genetic forms of autism may lead to similar patterns in brain activity and behavior. The findings were recently published in Nature Neuroscience.
Using brain-recording technology, the research team observed neurons across the entire brain to explore whether different genetic forms of autism share patterns and establish commonalities in neural responses. They found that, despite genetic differences, various forms may show a similar unique pattern of brain activity —also known as a brain signature.
“We hope this research will serve as a stepping stone linking genetic differences and behavioral atypicalities,” said Jean-Paul Noel, Ph.D., an assistant professor at the University of Minnesota Medical School.

