David Pearce — The Anatomy of Happiness
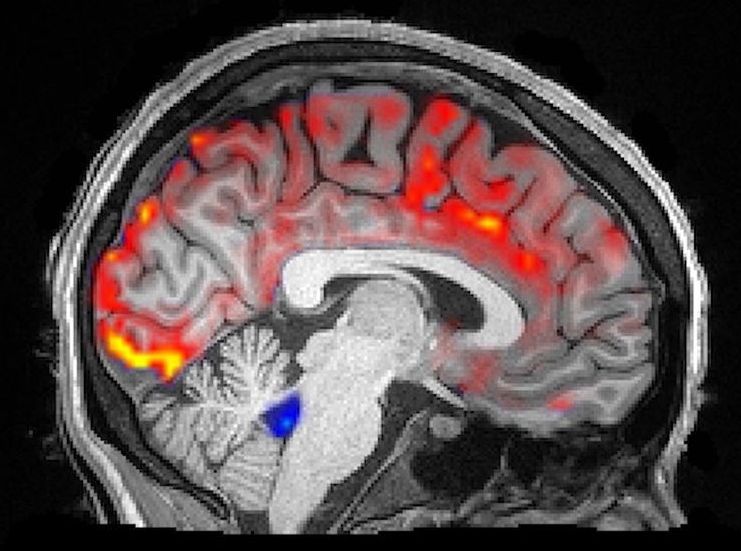
“While researching epilepsy, neuroscientist Itzhak Fried stumbled on a ‘mirth’ center in the brain — given this, what ought we be doing to combat extreme suffering and promote wellbeing?”
David Pearce — The Anatomy of Happiness… While researching epilepsy, neuroscientist Itzhak Fried stumbled on a ‘mirth’ center in the brain — given this, what ought we be doing to combat extreme suffering and promote wellbeing?
If one finds oneself viscerally hostile to the idea of universal happiness, and if by contemporary standards one falls within the statistically normal range in one’s emotional repertoire, then just how seriously should one contemplate the following possibility? Today we are the victims of what our successors will reckon an atavistic mood disorder. This disorder infects all our thoughts as well as all our feelings and volitions. It is a historical condition no less epistemically defective than are dream-psychoses from the perspective of the waking state.
Is the worry one might be locked in such an affective psychosis just the product of idle scepticism? Given the cognitive inaccessibility of most of the generically ecstatic states alluded to here, perhaps one wouldn’t know if one were so afflicted. After all, damaged and disfigured minds may have limited self-insight. Nor would one necessarily have the conceptual resources even to grasp what was at stake if one suffered from such a neural deficit. Pure, “unearned”, genetically-driven bliss of even the mildest flavour detracted from the inclusive fitness of one’s genes in the ancestral environment. Constitutionally happy freaks-of-nature got eaten or outbred. Hence unipolar euphoric mania today is vanishingly rare; unipolar melancholic depression and chronic dysthymia are all too common. Is one’s potential unease, if not revulsion, at the prospect of paradise-on-earth an incidental cultural by-product of natural selection? Or has selection pressure ensured that one is genetically predisposed to be biased against the idea of enduring bliss in the first instance?