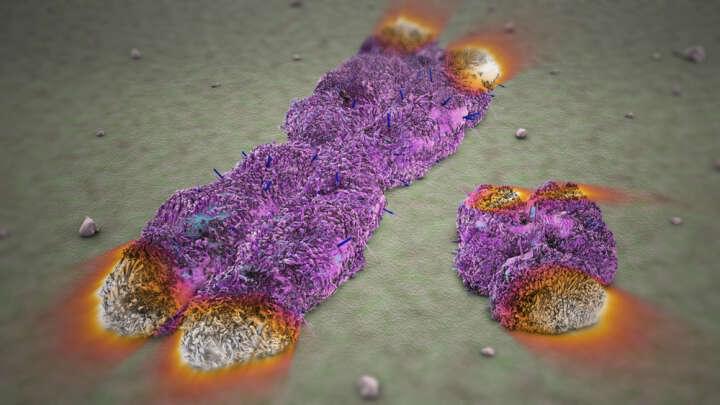
Telomeres are “caps” of non-coding DNA sequences present at both tips of our chromosomes, which are extremely important in the aging process. These caps protect our DNA as cells go through various life cycles of replication, however, each time a cell divides these telomeres are shortened and eventually contribute to disease and cellular aging.
Now, exciting new research published in the Journal PNAS has shown that an experimental gene therapy could be used to halt the shortening of these telomere caps in mice and by doing so increase the life span of these animals by up to 41 percent compared to controls.
Telomere length can be considered a marker of biological age and its shortening is a hallmark of a process called cellular senescence, which limits the replication of DNA in old damaged cells. As we age, telomere caps become shorter and shorter until the cell’s DNA becomes vulnerable to damage by cellular stresses that could lead to diseases such as cancer. Or the cell could ultimately reach senescence where it will no longer be able to replicate and so contribute to the aging process. For scientists looking at how to slow or even reverse aging, telomeres are of great interest.