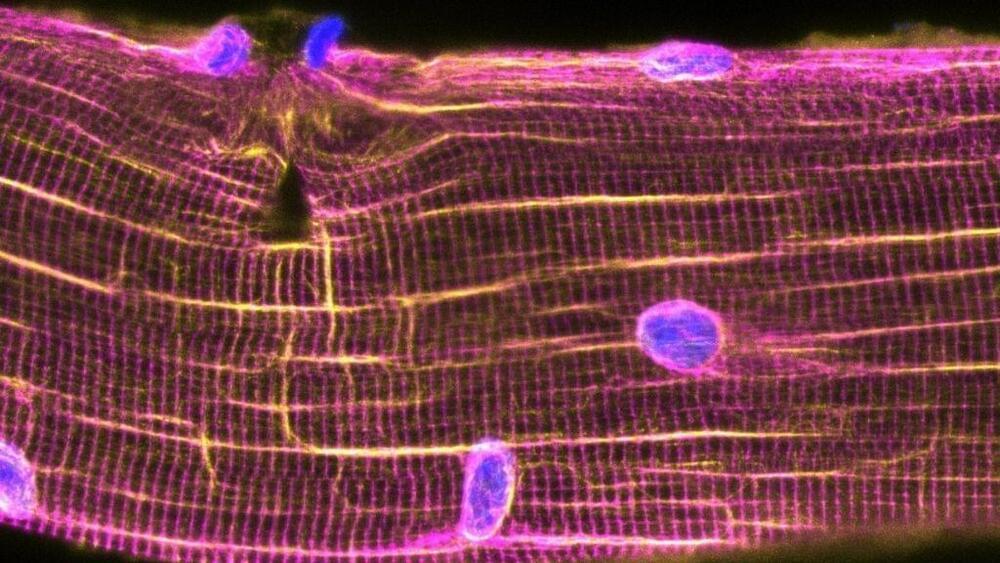
Exercise leaves muscles riddled with microscopic tears, so after a rigorous workout, the control centers of muscle cells — called nuclei — scoot toward these tiny injuries to help patch them up, scientists recently discovered.
In the new study, published Oct. 14 in the journal Science, researchers uncovered a previously unknown repair mechanism that kicks in after a run on the treadmill. Striking images show how, shortly after the exercise concludes, nuclei scuttle toward tears in the muscle fibers and issue commands for new proteins to be built, in order to seal the wounds. That same process likely unfolds in your own cells in the hours after you return home from the gym.