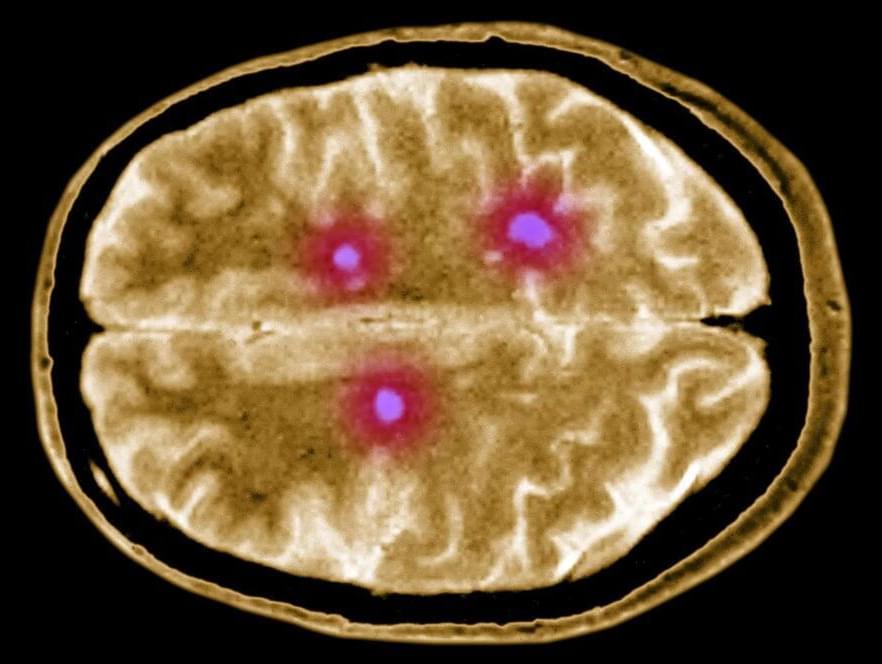
Research indicates enhanced mental function in individuals who maintain an active lifestyle and engage in social interactions, alongside managing blood pressure and diabetes effectively.
As federal approval for more Alzheimer’s disease medications progresses, a recent study conducted by UC San Francisco and Kaiser Permanente Washington reveals that tailored health and lifestyle modifications can postpone or prevent memory deterioration in older adults at increased risk.
The two-year study compared cognitive scores, risk factors, and quality of life among 172 participants, of whom half had received personalized coaching to improve their health and lifestyle in areas believed to raise the risk of Alzheimer’s, such as uncontrolled diabetes and physical inactivity. These participants were found to experience a modest boost in cognitive testing, amounting to a 74% improvement over the non-intervention group.