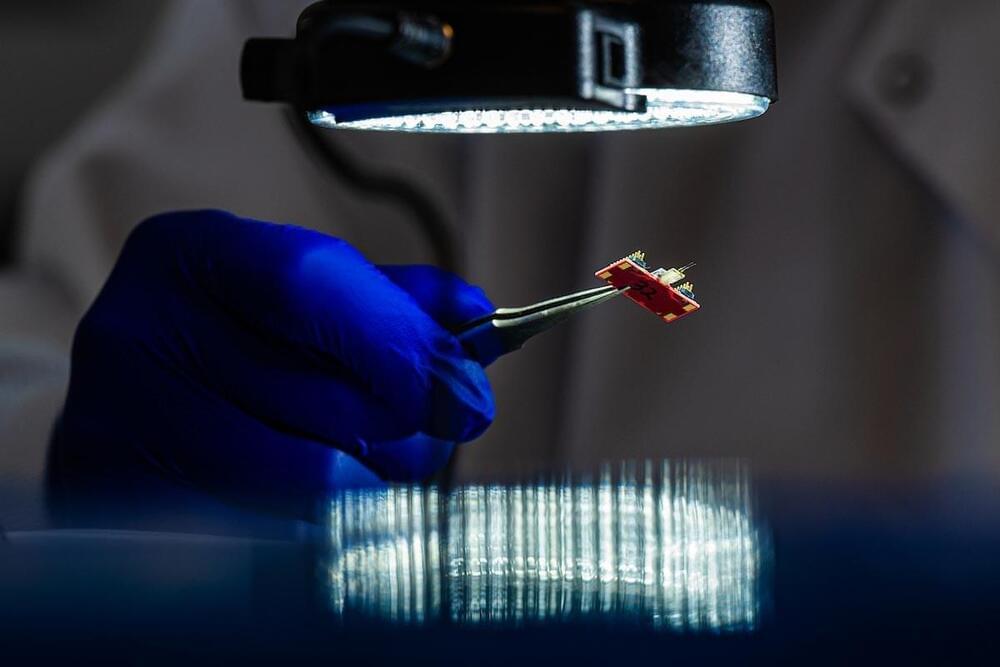
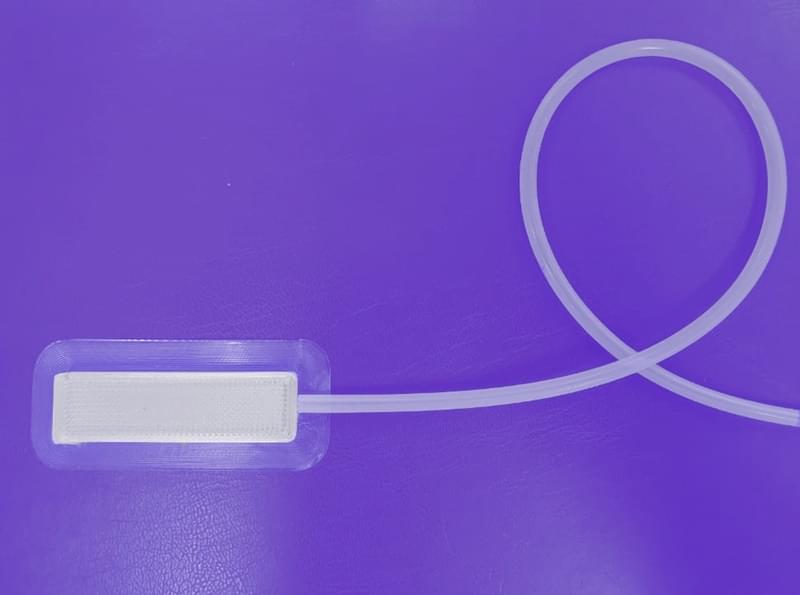
Rice University researchers have developed a new implantable sensor, spinalNET, capable of recording the electrical activity of spinal neurons in freely moving subjects. This breakthrough could help unlock the complexities of how spinal neurons process sensory and motor functions, potentially leading to better treatments for spinal cord diseases and injuries.
Implantable technologies have significantly improved our ability to study and even modulate the activity of neurons in the brain. However, neurons in the spinal cord are harder to study in action.
“If we understood exactly how neurons in the spinal cord process sensation and control movement, we could develop better treatments for spinal cord disease and injury,” said Yu Wu, a research scientist who is part of a team of Rice University neuroengineers working on a solution to this problem.