The accumulation of mutations in DNA is often mentioned as an explanation for the aging process, but it remains just one hypothesis among many. A team from the University of Geneva (UNIGE), in collaboration with the Inselspital, University Hospital of Bern and the University of Bern (UNIBE), has identified a mechanism that explains why certain organs, such as the liver, age more rapidly than others.
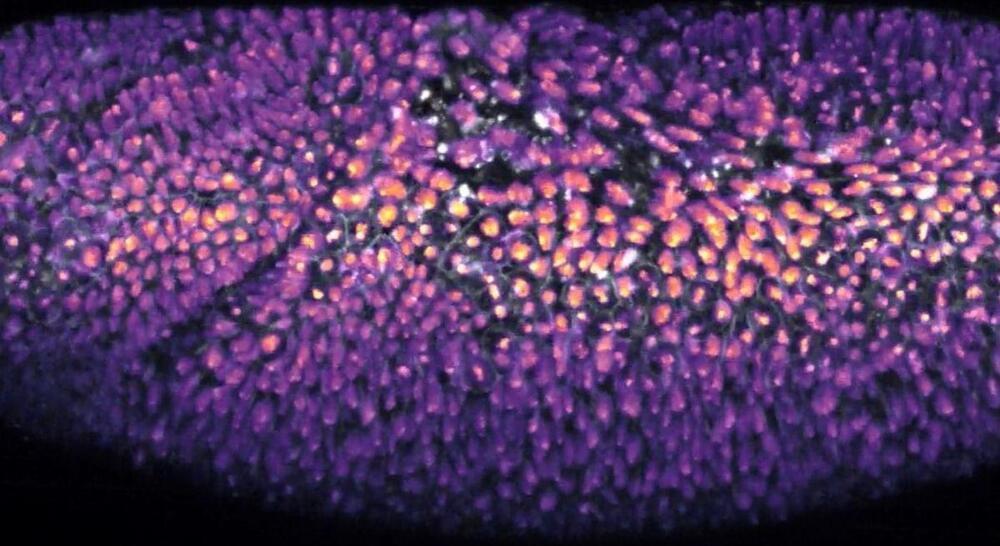
The mechanism reveals that damages to non-coding DNA, which are often hidden, accumulate more in slowly proliferating tissues, such as those of the liver or kidneys. Unlike in organs that regenerate frequently, these damages remain undetected for a long time and prevent cell division. These results, published in the journal Cell, open new avenues for understanding cellular aging and potentially slowing it down.
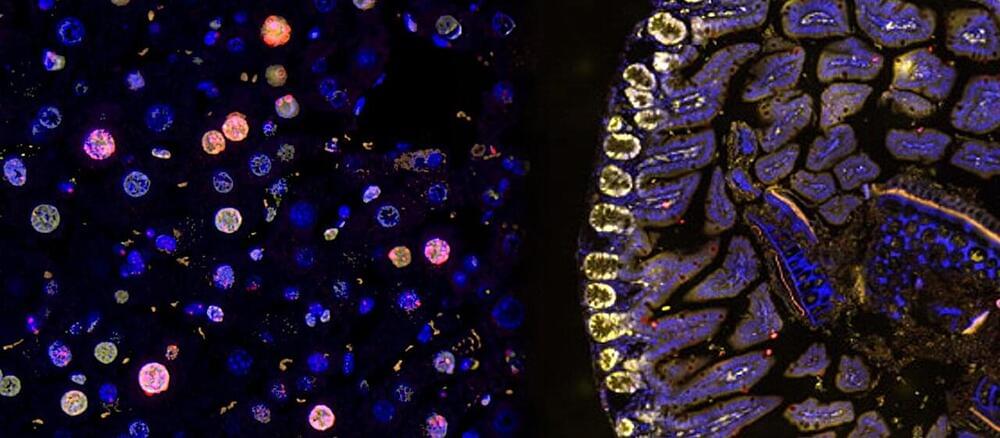
Our organs and tissues do not all age at the same rate. Aging, marked by an increase in senescent cells —cells that are unable to divide and have lost their functions—affects the liver or kidneys more rapidly than the skin or intestine.