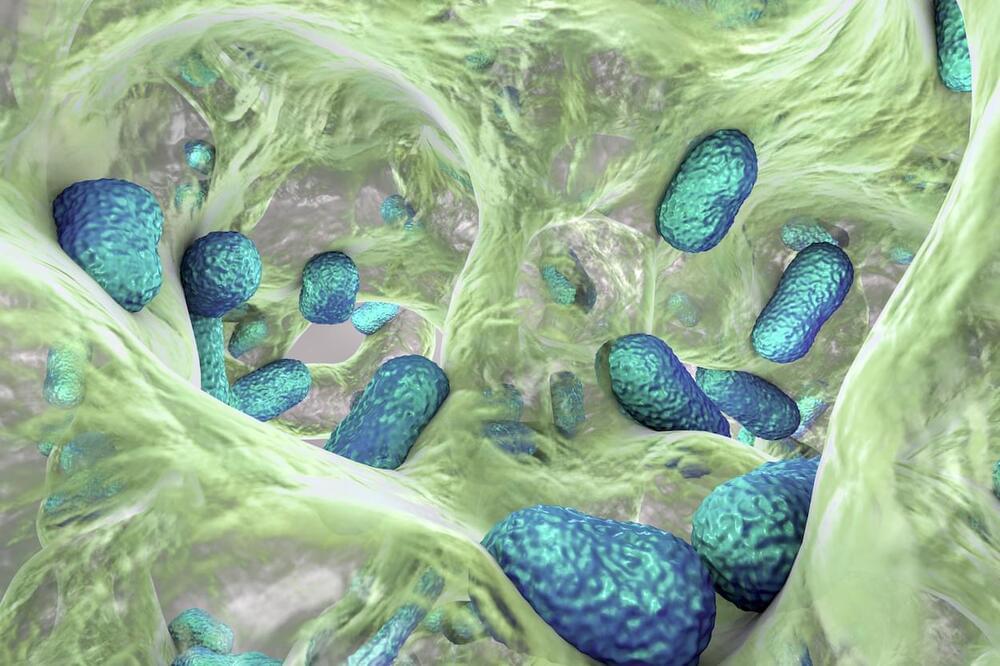
Stanford and McMaster University researchers created an artificial intelligence (AI) model to design molecules that inhibit the growth of Acinetobacter baumannii, a common drug-resistant bacteria. They synthesized and validated six structurally novel molecules that demonstrated antibacterial activity against A. baumannii and other phylogenetically diverse bacterial pathogens. This study represents a significant step toward the practical application of generative AI approaches for antibiotic discovery and drug discovery in general.
The research article, “Generative AI for designing and validating easily synthesizable and structurally novel antibiotics,” was published in Nature Machine Intelligence.
Among the most critical issues in contemporary medicine is the worldwide spread of factors contributing to antibiotic resistance. In 2019, drug-resistant infections were responsible for an estimated 4.95 million deaths. As new antibiotics are being developed slower than the spread of antimicrobial resistance determinants, this figure is expected to reach 10 million annually by 2050.

 עברית (Hebrew)
עברית (Hebrew)