Neuroscientists have established in recent decades the idea that some of each day’s experiences are converted by the brain into permanent memories during sleep the same night. Now, a new study proposes a mechanism that determines which memories are tagged as Important enough to linger in the brain until sleep makes them permanent.
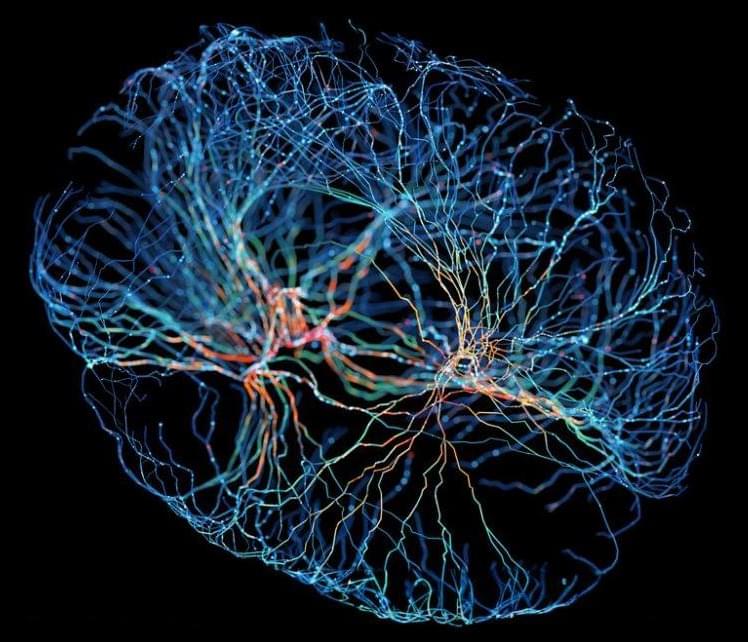
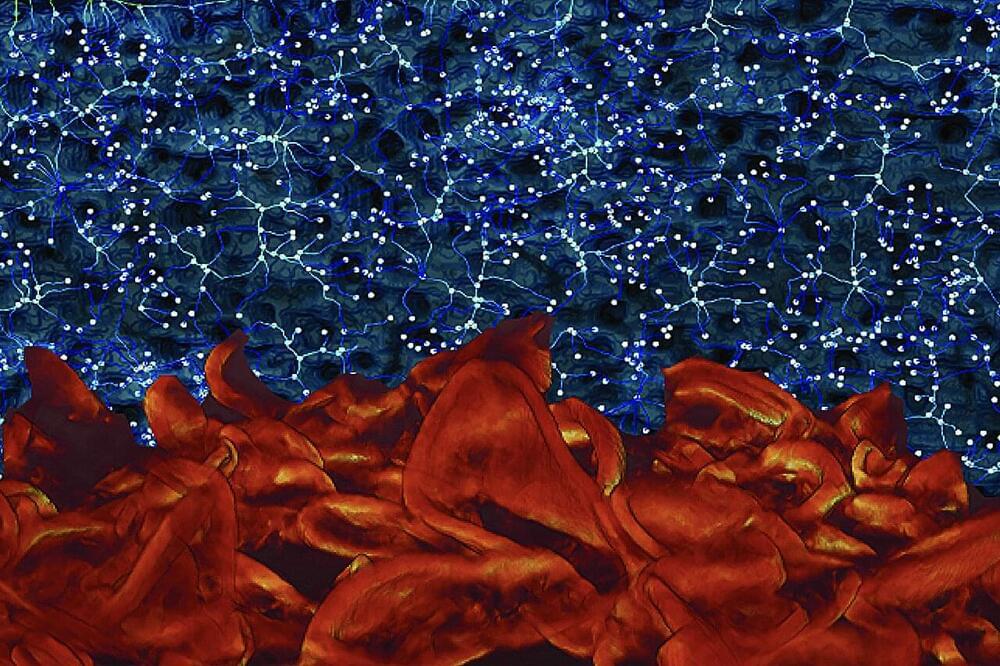
Led by researchers from NYU Grossman School of Medicine, the study revolves around brain cells called neurons that “fire” – or bring about swings in the balance of their positive and negative charges — to transmit electrical signals that encode memories. Large groups of neurons in the hippocampus fire together in rhythmic cycles, creating sequences of signals within milliseconds of each other that can encode complex information.
Called “sharp wave-ripples,” these “shouts” to the rest of the brain represent the near-simultaneous firing of 15 percent of hippocampal neurons, and are named for the shape they take when their activity is captured by electrodes and recorded on a graph.