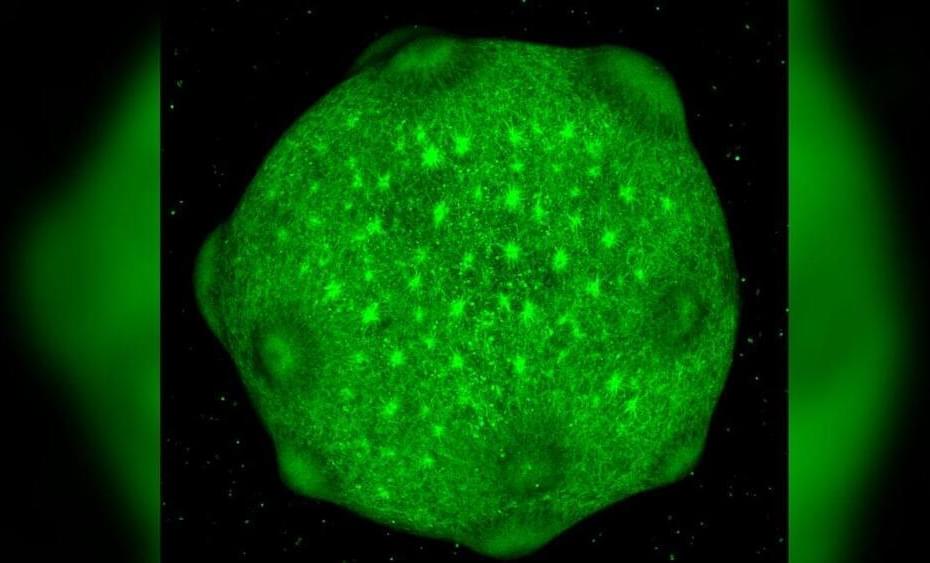
In a study published in Cell Reports Physical Science (“Electro-Active Polymer Hydrogels Exhibit Emergent Memory When Embodied in a Simulated Game-Environment”), a team led by Dr Yoshikatsu Hayashi demonstrated that a simple hydrogel — a type of soft, flexible material — can learn to play the simple 1970s computer game ‘Pong’. The hydrogel, interfaced with a computer simulation of the classic game via a custom-built multi-electrode array, showed improved performance over time.
Dr Hayashi, a biomedical engineer at the University of Reading’s School of Biological Sciences, said: Our research shows that even very simple materials can exhibit complex, adaptive behaviours typically associated with living systems or sophisticated AI.
This opens up exciting possibilities for developing new types of ‘smart’ materials that can learn and adapt to their environment.