Veritaco CEO Jeffrey Bowie faces charges for allegedly installing malware on hospital computers, violating Oklahoma’s Computer Crimes Act.



Synchron has developed a Brain-Computer Interface that uses pre-existing technologies such as the stent and catheter to allow insertion into the brain without the need for open brain surgery.
Read the CNET article for more info:
You Might Not Need Open Brain Surgery to Get Mind Control https://cnet.co/3sZ7k67
0:00 Intro.
0:25 History of Brain Chip Implants.
0:44 About Synchron.
0:54 How Synchron implants the interface.
1:55 How brain patterns transmit signals.
2:50 Risks and Concerns.
3:50 Patients and Clinical Testing.
4:25 Brain Health Monitoring.
5:04 Synchron Switch Price.
Never miss a deal again! See CNET’s browser extension 👉 https://bit.ly/3lO7sOU
Check out CNET’s Amazon Storefront: https://www.amazon.com/shop/cnet?tag=lifeboatfound-20.
Follow us on TikTok: / cnetdotcom.
Follow us on Instagram: / cnet.
Follow us on Twitter: / cnet.
Like us on Facebook: / cnet.
#WhatTheFuture #Synchron #BCI
Improving the human brain with the help of implanted chips and AI: Elon Musk’s startup Neuralink is among the companies developing this tech. Initial tests show it could be a game changer for people with disabilities.
#technology #braincomputerinterface #bci #australia #medicine #optimization #elonmusk #neuralink #stentrode #brain #computer #dishbrain.
▸ subscribe to our channel: https://goo.gl/UupwgM

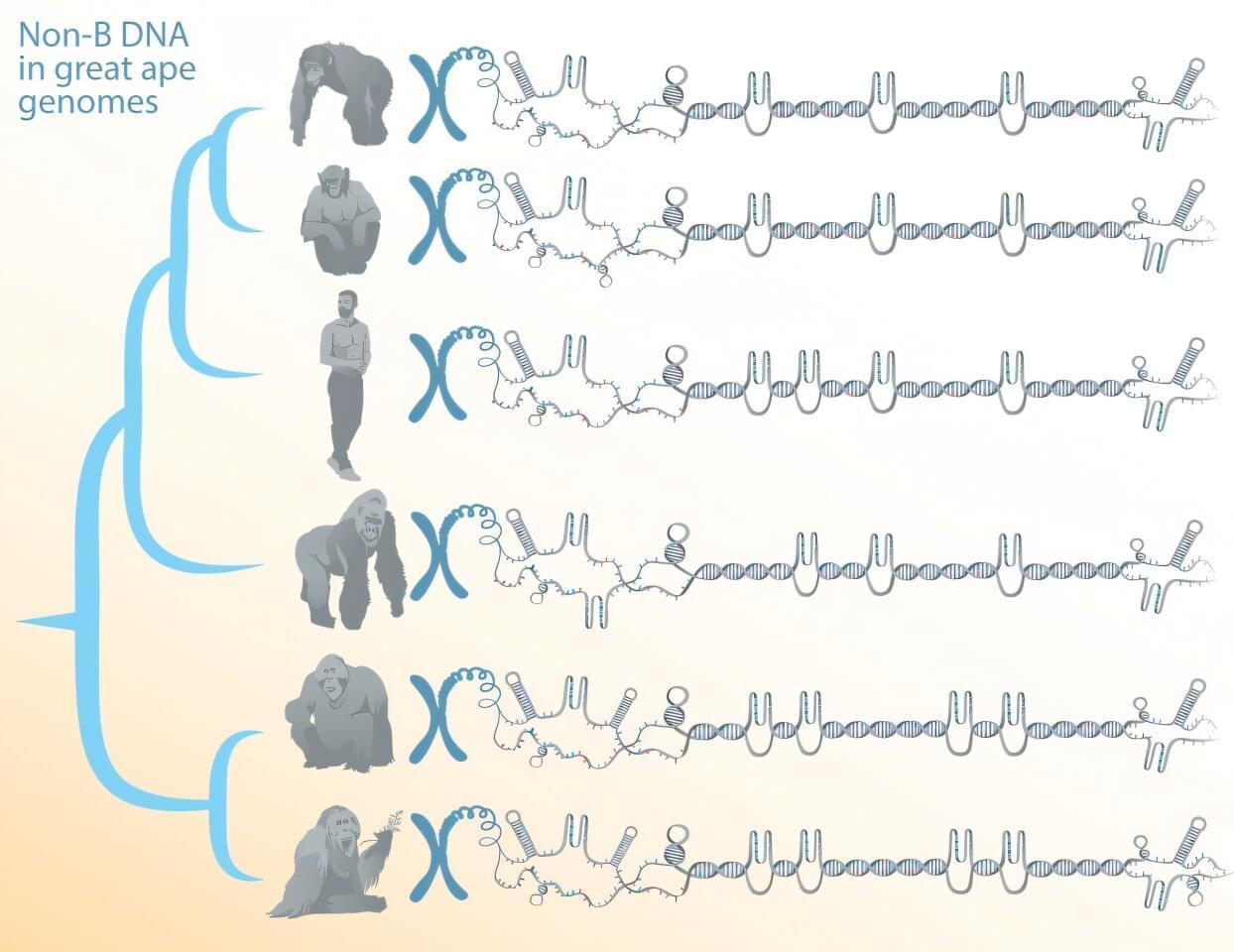
Certain DNA sequences can form structures other than the canonical double helix. These alternative DNA conformations—referred to as non-B DNA—have been implicated as regulators of cellular processes and of genome evolution, but their DNA tends to be repetitive, which until recently made reliably reading and assembling their sequences difficult.
Now, a team of researchers, led by Penn State biologists, has comprehensively predicted the location of non-B DNA structures in great apes. It’s the first step in understanding the functions and evolution of such structures, known to contribute to genetic diseases and cancer, the team said.
The work depends on newly available telomere-to-telomere (T2T), or end-to-end, genomes of humans and other great apes that overcame sequencing and assembly difficulties associated with repetitive DNA to fill in any remaining gaps in the genomes. A paper describing the study, which shows that non-B DNA is enriched in the newly sequenced segments of the genomes and suggests potential new functions, was published in the journal Nucleic Acids Research.

Patients in the early stages of psychosis respond to treatments differently than those who have developed a chronic version of the disorder. Understanding the neurobiological changes from early to chronic stages is essential for developing targeted prevention and treatment strategies. But how symptoms change during this transition—and what role the brain plays—is unclear.
Researchers at Yale School of Medicine (YSM) have now examined patients with early and chronic forms of psychosis to map symptom evolution and identify relevant brain networks. They published their findings in the journal Neuropsychopharmacology.
“We are interested in how psychosis and psychiatric disorders develop,” says Maya Foster, first author of the study and a Ph.D. student in the lab of Dustin Scheinost, Ph.D., associate professor of radiology and biomedical imaging at YSM.