It turns out the gut is full of surprises. And one of those surprises may have offered up a key for unlocking a new way of treating multiple sclerosis (MS). Investigators from Brigham and Women’s Hospital have discovered a microRNA—a small RNA molecule—that increases during peak disease in a mouse model of MS and in untreated MS patients. When a synthetic version of the microRNA was orally given to the mice, it prevented disease. While several steps remain before these insights can be translated into therapy for patients, the researchers describe their results as both exciting and unexpected. Their findings are published in Cell Host & Microbe.
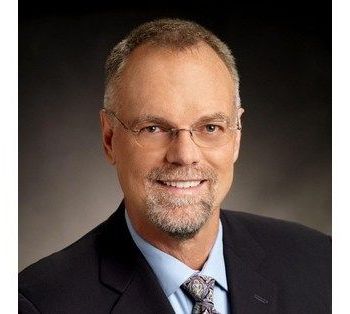
“We’ve discovered a new mechanism to regulate the microbiome and treat human disease that hadn’t been known before,” said senior author Howard Weiner, MD, co-director of the Ann Romney Center for Neurologic Diseases at the Brigham. “The gut microbiome is known to play an important role in MS and other diseases. Our findings, which show that a microRNA can be used to target and influence the microbiome with precision, may have applicability for MS and many other diseases, including diabetes, ALS, obesity and cancer.”
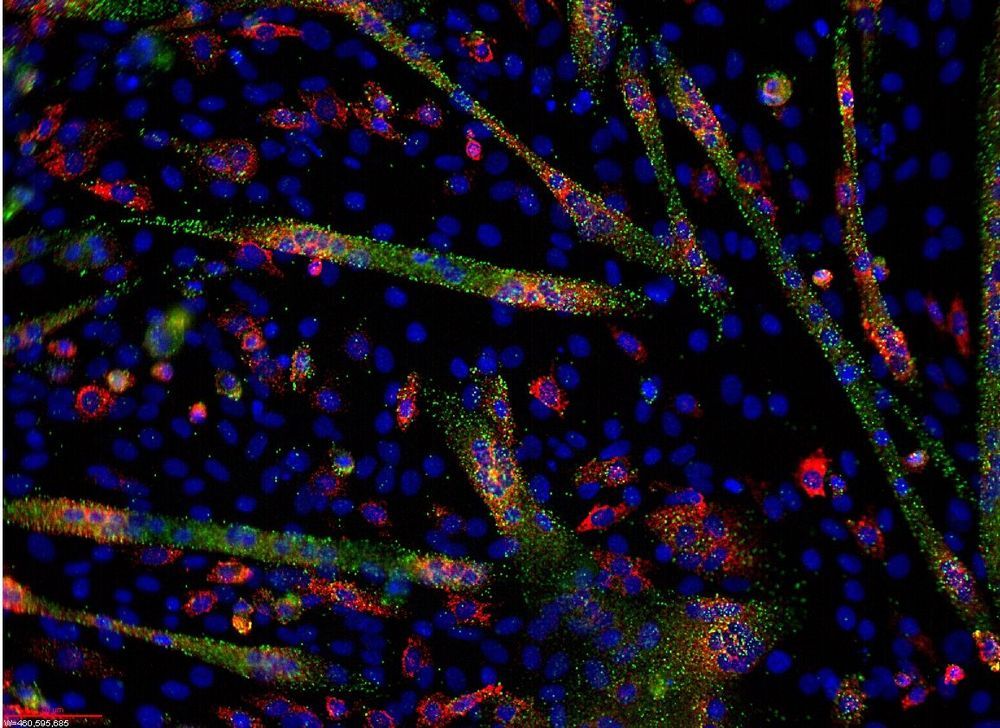
Weiner, lead author Shirong Liu, MD, Ph.D., an instructor in the Weiner laboratory, and their colleagues investigated how the altered gut microbiome affects the course of MS. To do so, they studied the microbiome and microRNAs found in the experimental autoimmune encephalomyelitis (EAE) model of MS. Unexpectedly, they found that when they transferred fecal matter from EAE mice at peak disease, it protected the mice who received the transfer. The team found that a specific microRNA, known as miR-30d, rather than live bacteria, was responsible for preventing disease. The investigators found that miR-30d is enriched in untreated, relapsing-remitting MS patients as well.