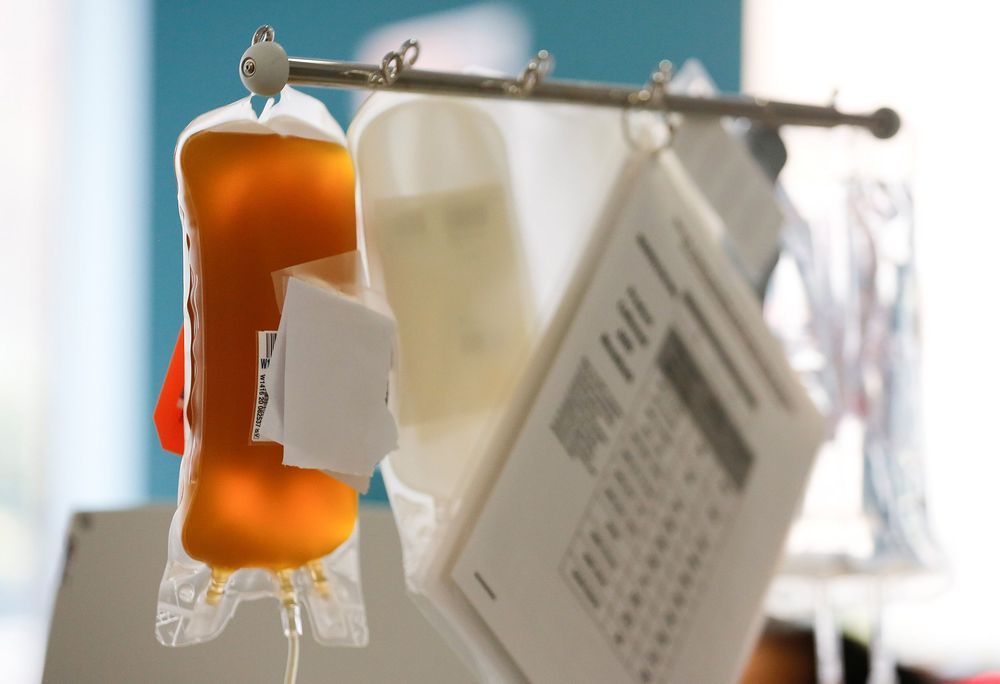
Paris (AFP) — An antibody from a patient who recovered from SARS has been shown to block COVID-19 infection in a laboratory setting, researchers said Monday in another potential breakthrough in the search for coronavirus treatment.
Scientists based in Switzerland and the United States previously isolated the antibodies from the patient in 2003, following the SARS outbreak that killed 774 people.
They experimented with 25 different types of antibodies — which target specific protein spikes on viruses — to see if they could prevent cells becoming infected with COVID-19.