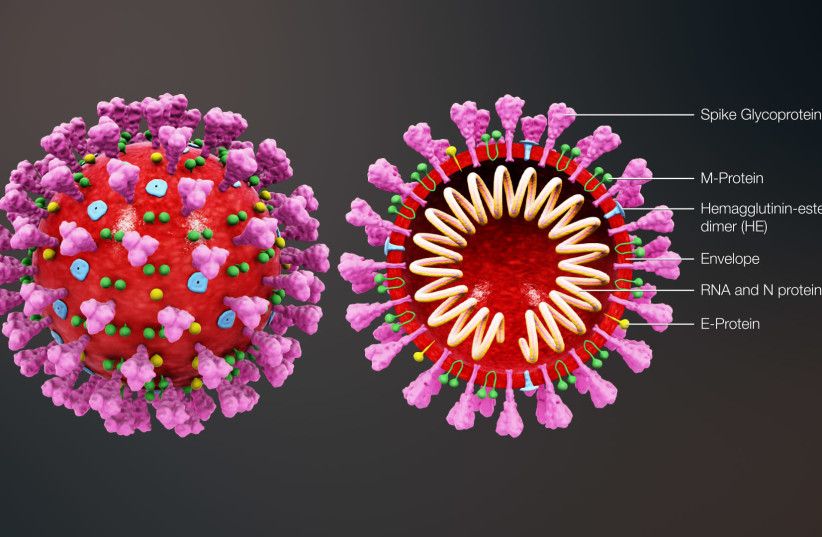
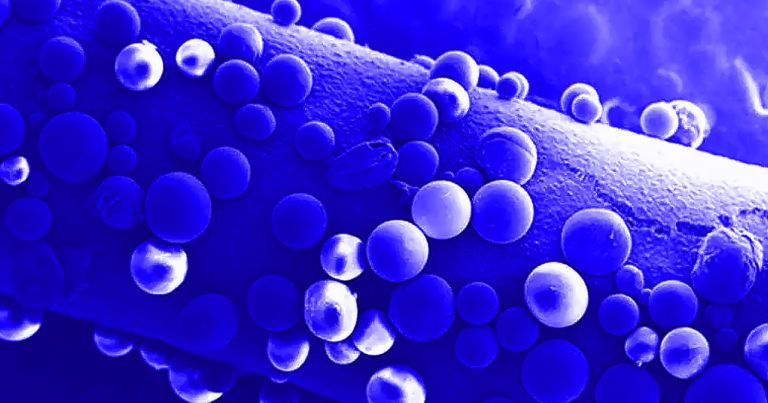
Essentially, the study found that some immune systems are less capable of recognizing the infection. This diminished ability to recognize the coronavirus can make a person more susceptible to developing symptoms in general, as well as more likely to experience severe symptoms that require hospitalization.
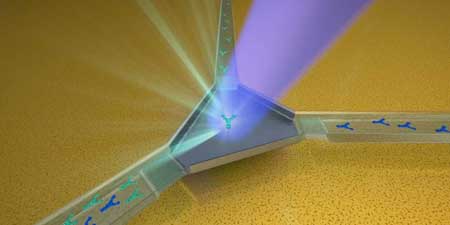
Getting down to the scientific specifics of the findings, the study focused on the immune system genes known as human leukocyte antigen genes. These genes are highly involved in the immune system’s ability to recognize pathogens, but they come in a variety of forms and vary from person to person.
The research team, from Oregon Health & Science University and the Portland VA Research Foundation, believe that HLA gene variations may make certain people more vulnerable to the coronavirus.