A groundbreaking advancement in the field of vision restoration has recently emerged from the intersection of nanotechnology and biomedical engineering. Researchers have developed a novel retinal prosthesis constructed from tellurium nanowires, which has demonstrated remarkable efficacy in restoring vision to blind animal models. This innovative approach not only aims to restore basic visual function but also enhances the eye’s capability to detect near-infrared light, a development that holds promising implications for future ocular therapies.
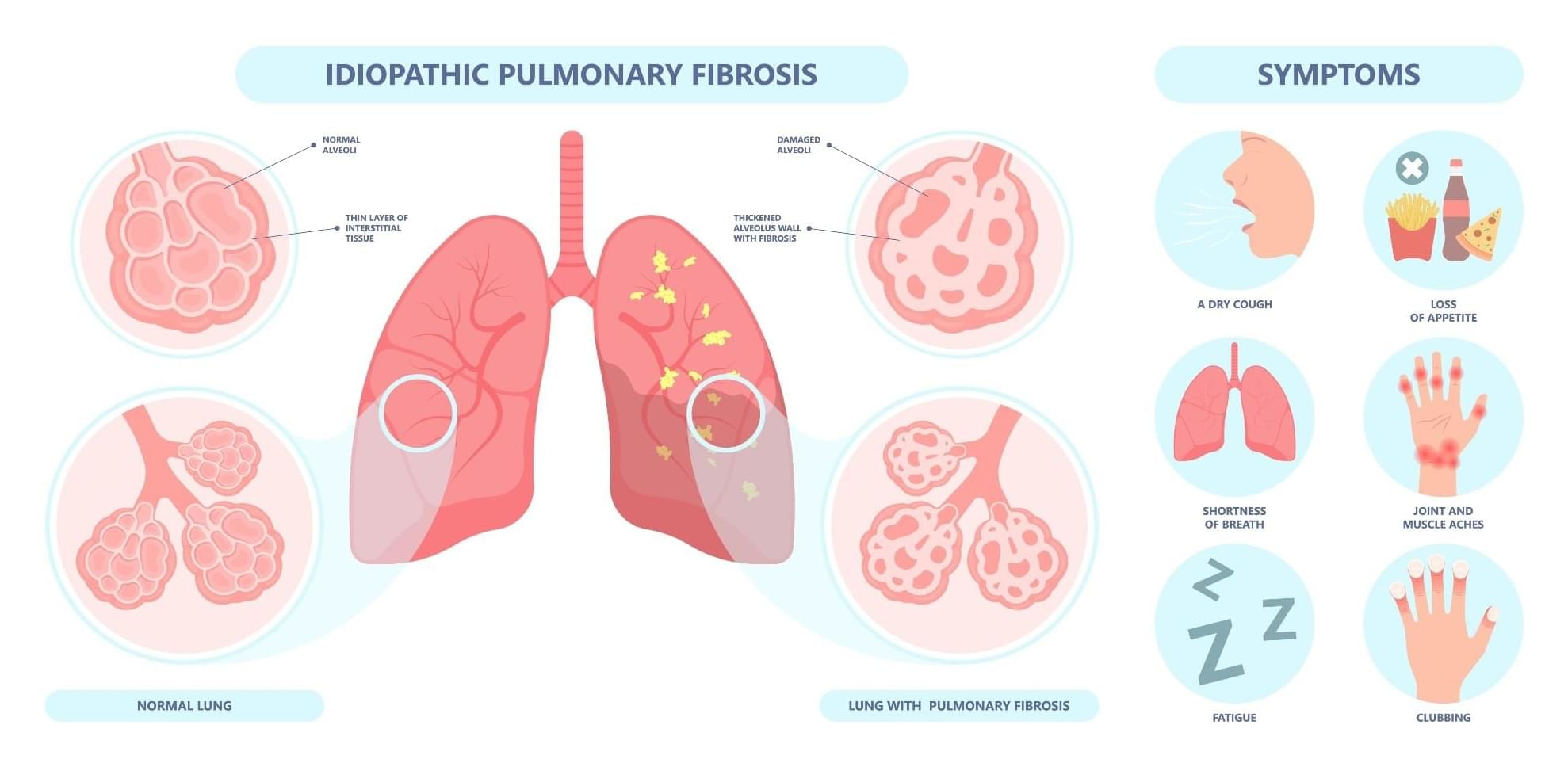
The retina, a thin layer of tissue at the back of the eye, plays a crucial role in converting light into the electrical signals sent to the brain. In degenerative conditions affecting the retina, such as retinitis pigmentosa or age-related macular degeneration, this process is severely disrupted, ultimately leading to blindness. Traditional treatments have struggled with limitations such as electrical interference and insufficient long-term impacts. However, the introduction of a retinal prosthesis made from tellurium offers a fresh perspective on restoring vision.
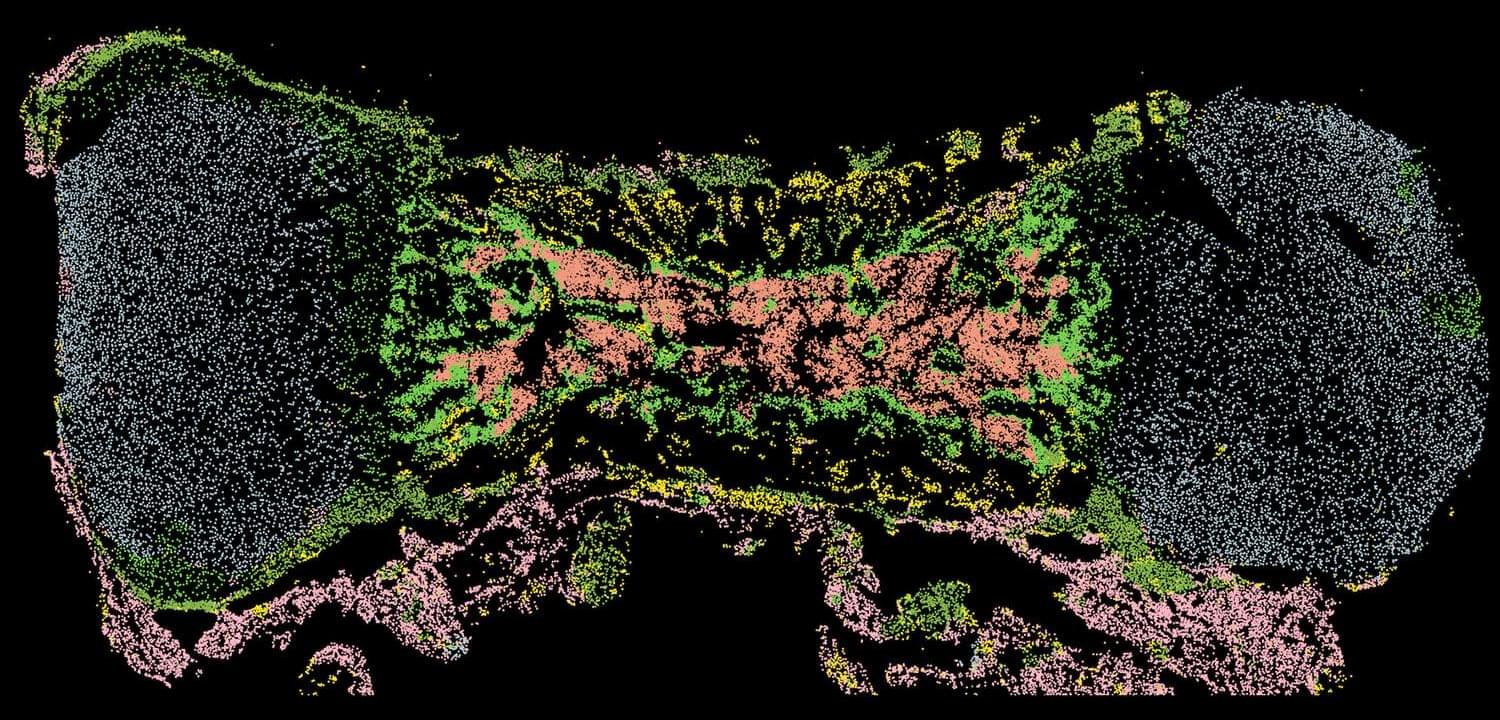
Tellurium is a unique element known for its semiconductor properties, making it an excellent choice for developing nanostructured devices. The researchers carefully engineered tellurium nanowires and then integrated them into a three-dimensional lattice framework. This novel architecture facilitates easy implantation into the retina while enabling efficient conversion of both visible and near-infrared light into electrical impulses. By adopting this approach, the researchers ensured that the prosthesis would function effectively in various lighting conditions, a significant consideration for practical application in real-world scenarios.