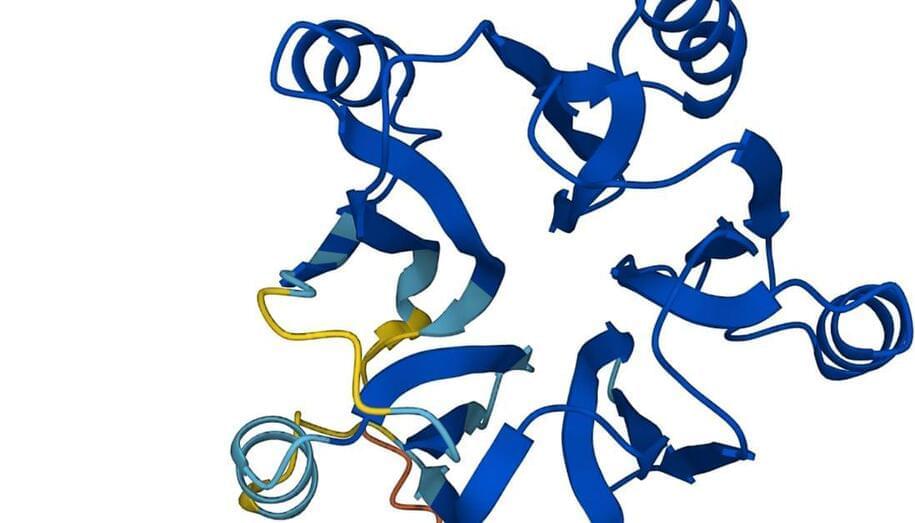
Got a protein? This AI will tell you what it looks like.
AlphaFold was recognized by the journal Science as 2021’s Breakthrough of the Year, beating out candidates like Covid-19 antiviral pills and the application of CRISPR gene editing in the human body. One expert even wondered if AlphaFold would become the first AI to win a Nobel Prize.
The breakthroughs have kept coming.
Last week, DeepMind announced that researchers from around the world have used AlphaFold to predict the structures of some 200 million proteins from 1 million species, covering just about every protein known to human beings. All of that data is being made freely available on a database set up by DeepMind and its partner, the European Molecular Biology Laboratory’s European Bioinformatics Institute.